Greetings anatomy students! Whew! Nine weeks have elapsed since our first eye lesson and today marks the final installment about the effective, efficient, elegant eye. So, welcome to today’s Anatomy Lesson #33, EyeMax – The Eye – Part 5.
The lesson contains some fun tests to perform with our eyes. You know the drill: try this – try that. It also includes possible spoiler alerts with excerpts from two of Diana’s later books; as always, no names, no dates, and no places are revealed.
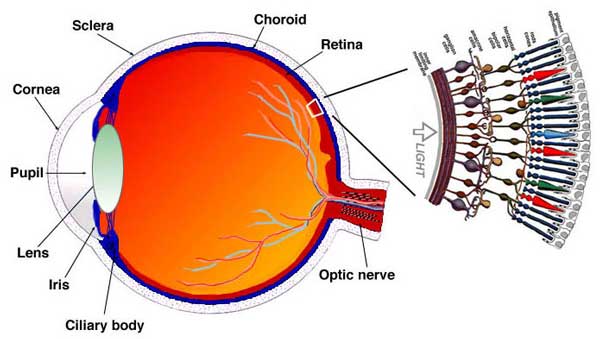
Let’s begin where we left off with The Eye – Part 4. We have already covered most eye structures so today we will finish with two humors of the globe, retina and visual centers of the brain.
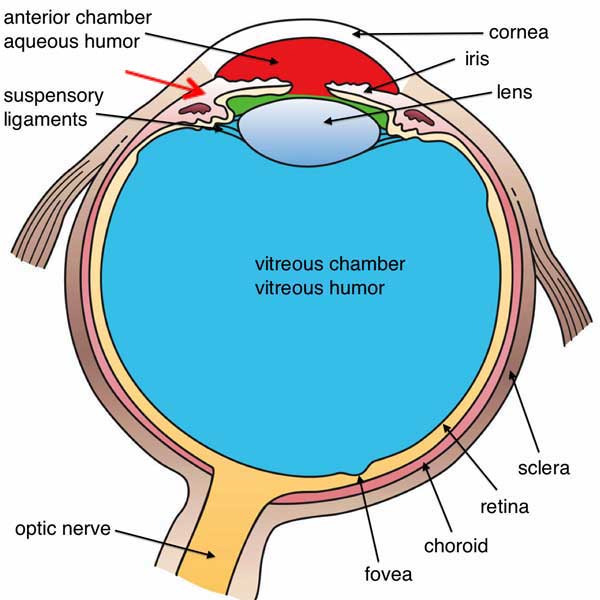
You may recall that the eyeball has three important chambers: anterior chamber between iris and cornea (Photo A, red area); posterior chamber between iris, lens and suspensory ligaments (Photo A, green area); and the large vitreous chamber behind the lens (Photo A, blue area). You may also recall the ciliary body (Photo A, red arrow); it contains the ciliary muscle, attaches to suspensory ligaments/zonular fibers (Anatomy Lesson #32), and produces aqueous humor (humour).
Photo A
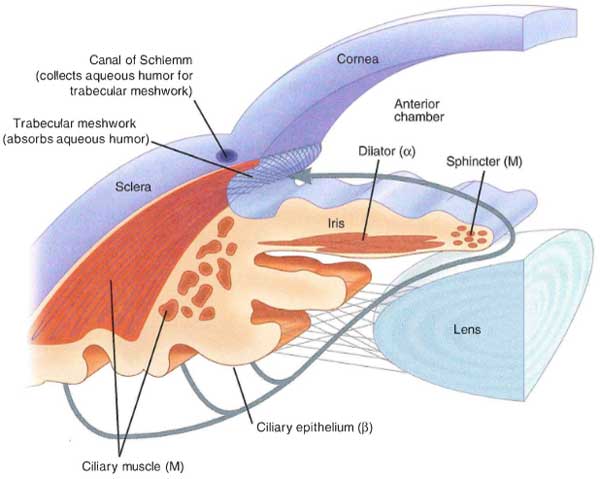
As watery aqueous humor is made by the ciliary body, it collects in the posterior chamber and then flows forward through the pupil into the anterior chamber (Photo B). A spongy trabecular meshwork fills the angle between cornea and iris (Photo B) and contains the canal of Schlemm, a circular lymphatic-like vessel. From the anterior chamber, aqueous humor drains into the canal of Schlemm and from there into the venous system. A normal eye produces and absorbs about 3-4 ml (~¾ tsp.) of aqueous humor every 24 hours; a delicate balancing act thus exists between production and absorption of this fluid..
Aqueous humor serves two main purposes; it provides oxygen and nutrients to parts of the avascular lens and cornea and it assists the corneal refraction of light rays.
Photo B
For those preferring a video, this gif shows production and absorption of aqueous humor:
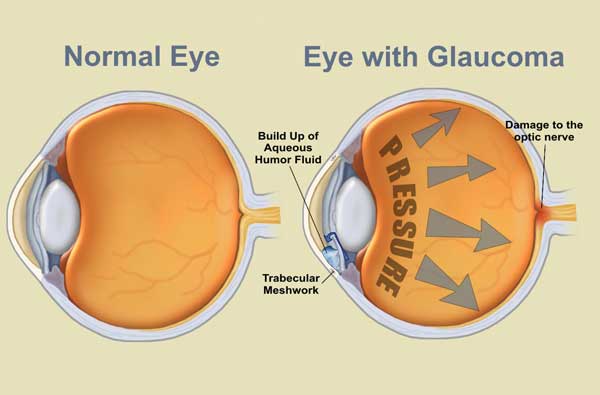
But, sometimes the unthinkable happens and production of aqueous humor outstrips absorption. The eye is a closed system (no external opening), so if aqueous humor builds up, then intraocular pressure (IOP) rises. Known as glaucoma, this condition must be diagnosed and controlled with medication or surgery (or both) otherwise the optic nerve may be damaged resulting in decreased vision or blindness. Understand that glaucoma is not a single condition, rather, there are several different types of glaucoma.
POSSIBLE SPOILER ALERT and Clinical Correlation #1: In Diana’s 6th book, A Breath of Snow and Ashes, our ever resourceful Claire treats a patient with an acute attack of closed-angle glaucoma (a true medical emergency)!
I had long suspected that the cause of (her) blindness was glaucoma—rising pressure inside the eyeball that if untreated eventually damages the optic nerve. She was plainly having an acute attack… I abstracted the largest needle, a three-inch length of steel… The left eye bulged noticeably beneath its lid, vividly bloodshot… With a quick prayer to Saint Clare—who was, after all, patroness of sore eyes, as well as my own patron saint—I ran the needle through the flame of the lamp, poured pure alcohol onto a rag, and wiped the soot from the needle. I shoved the needle hard into the sclera of the eye, near the edge of the iris.
Closed-angle glaucoma occurs because the Canal of Schlemm is blocked or does not drain properly so aqueous humor accumulates with a sudden and dramatic increase in IOP (Photo C). Although crude, Claire’s 18th century treatment (no access to modern medications and procedures!) released aqueous humor from the anterior chamber relieving IOP. Her treatment could not restore sight, but it could offer the patient temporary relief from horrific pain.
Photo C
The vitreous humor (vitreous body) is a transparent, avascular gelatinous mass occupying the vitreous chamber (see Photo A). Photo D is a model illustrating the vitreous as a blue mass marked by the black line. Vitreous humor is mostly water but other molecules lend it a gel-like consistency although it may liquefy with age. Unlike aqueous humor, the vitreous is not continuously renewed. Vitreous humor serves three important functions: it fills the globe augmenting its spherical shape, it secures the retina by pressing it against the choroid coat (see Photo A), and it helps refraction of light rays.
Photo D
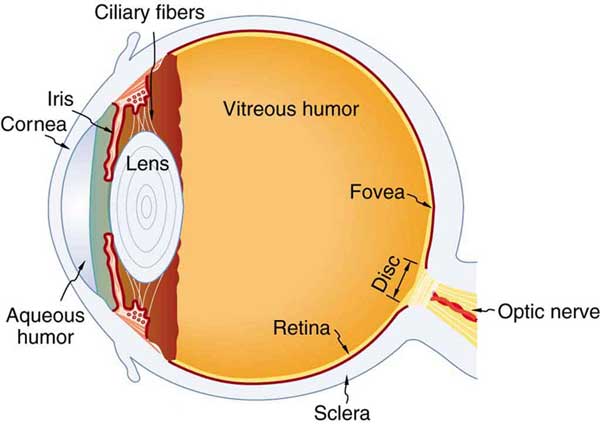
Now, let’s consider the complex retina and its parts. The extensive retina covers about 65% of the inner surface of the eyeball (Photo E – yellow layer).
Photo E
As an eye specialist peers into your eye via ophthalmoscope, the fundus or back of the eyeball is revealed. In everyday terms, the photographic red eye is a reflection of light from the fundus of the eye.
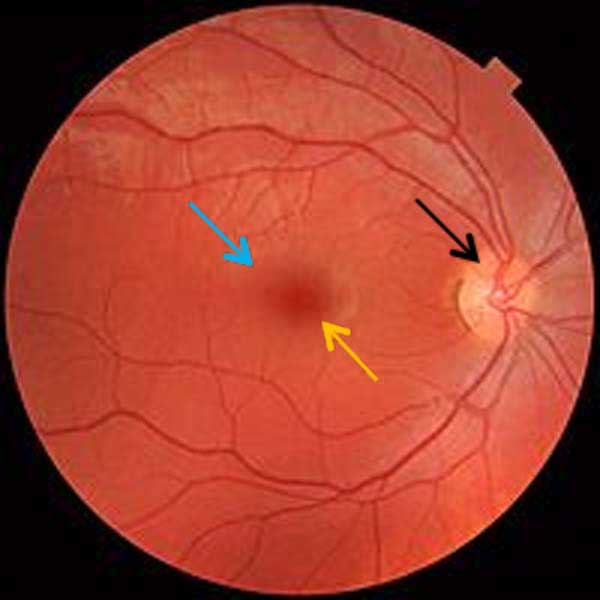
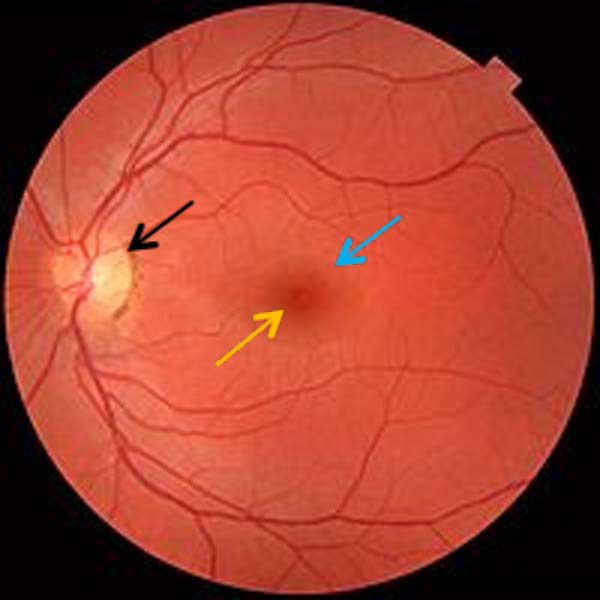
Viewing the fundus reveals the inner surface of the retina, an extension of the brain. Photo F is the fundus of a right eye and Photo G is the fundus of a left eye. Each black arrow points to the bright optic disc or blind spot, where the optic nerve (Cranial Nerve II) forms; sight is absent at the blind spot because it lacks photoreceptors (see below). Red branches emerging/converging at each optic disc are retinal vessels that provide oxygen and nutrients to or remove waste products from the inner retina. Blue arrows point to the maculae (pl.), pale regions each containing a dark central spot, the fovea (orange arrows). Each fovea contains the fovea centralis, a central pit marking the site of greatest visual acuity.
Fundic examination is important because it helps reveal the health of the retina; it is also the only site where the microcirculation (small blood vessels) can be observed and the only region where part of the brain can be seen directly without tissue disruption or intervention.
Clinical Correlation #2: Macular degeneration (MD) is a common disorder causing decreased visual acuity and even blindness. This condition is aptly named because retinal cells of the maculae are damaged along with other associated changes. There are several types of MD with various risk factors but the most common is age-related MD and it is considered incurable. As always, science presses onward and (mostly) upward! Last month London eye surgeons treated a British patient using a tiny patch of stem cell-derived tissue to successfully restore eyesight lost through macular degeneration!
Photo F
Photo G
Hey, hey, students! Are ye awake and paying attention? JAMMF is checkin’ ye out just to be sure!
Try this: Let’s test our blind spots the sites where optic nerves form. Close your left eye and stare with your right eye at the cross in Photo H. You should see the elephant in your peripheral vision but keep focused on the cross. If you can’t see the elephant, then move away from the screen until you can. While looking at the cross, slowly move closer to the screen. At about one foot (~ 31 cm) away from the cross, the elephant will disappear from view because its image is falling on your right blind spot! Now, for fun, close the right eye and stare at the elephant. Move in and out until the cross disappears; again, this happens because its image is falling on your left blind spot. Excellent job, students!
Photo H
Try this: Let’s test our fovea centrales (pl.) by staring at the words “Jamie and Claire” in the sentence below; these words should be crisp and clear because their images fall directly on the fovea centrales of our retinae (pl.), sites of greatest visual acuity. Notice that the remaining words of the sentence are unclear because their images fall elsewhere on the retinae where vision is less acute.
FANS ARE HEAD OVER HEELS FOR JAMIE & CLAIRE, OUR FAVORITE SI-FI CHARACTERS.
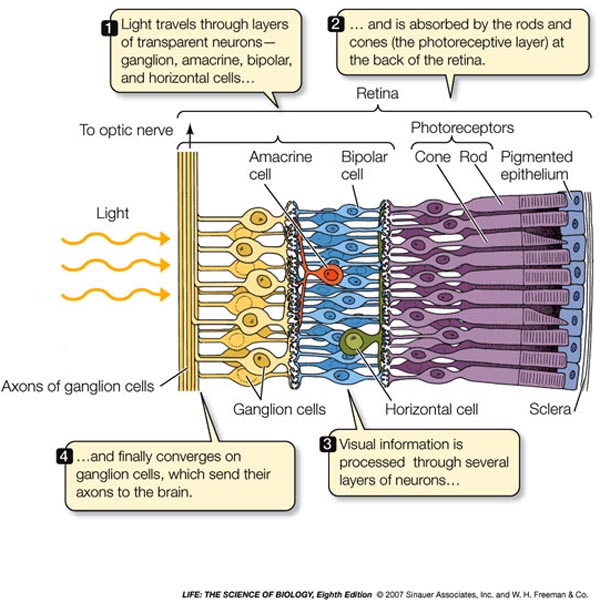
Returning to retinal anatomy Photo I (right side) shows an enlarged graphic representation of the retina. The retina has about 10 named layers, but for this lesson we will cover only three.
Photo I
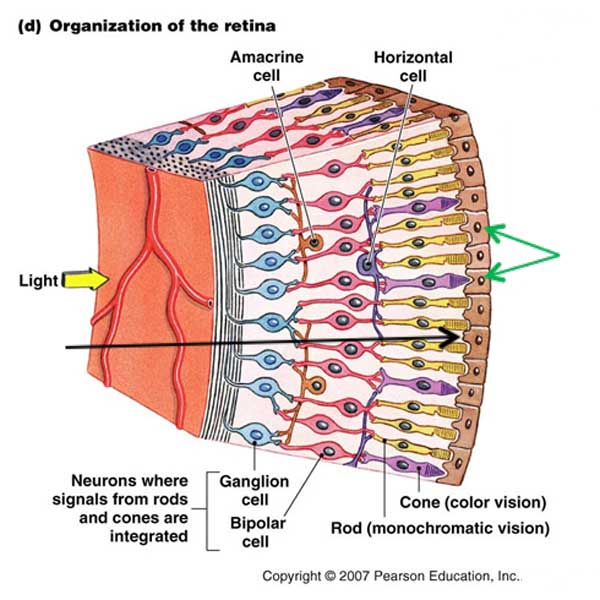
Photo J is a schematic of a wee bit of retina (cornea lies to the left). The yellow arrow shows light rays approaching the retina. The black arrow shows that light rays pass through the retina until they reach a layer of rods and cones, two types of photoreceptor cells. Some light rays bypass the rods and cones to reach the deeper retinal pigment epithelium or RPE (Photo J – green arrows). RPE contains brown melanin that absorbs extraneous light rays bypassing rods and cones and thus improving our quality of vision.
To the left of the RPE are the photoreceptive rods and cones. Cones (Photo J – lavender cells) are responsible for chromatic (color) vision. Rods (Photo J – yellow cells) are responsible for achromatic (non-color) vision. To the left of rods and cones are several other retinal cell types which we will not cover. However, the innermost layer are ganglion cells; their processes (axons) form the optic nerve (Photo J – blue cells).
Photo J
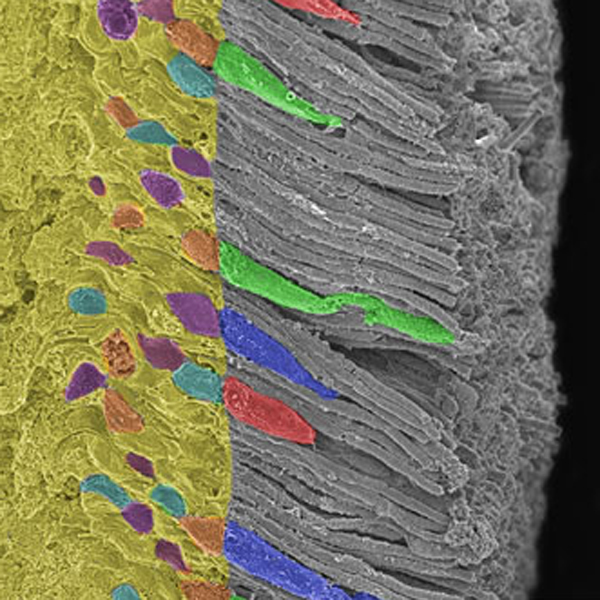
Photo K shows rod and cone cells by scanning electron microscopy (RPE is absent); the names derive from the shape of their outer segments. Rods cells have long, thin outer segments (Photo K – grey columns). Cone cells have cone-shaped outer segments (Photo K – artificially colored blue, green or red). Rod and cone outer segments contain photosensitive molecules that respond to light.
Each human retina contains about 120 million rod cells that are absent from the fovea but increase in numbers away from the fovea. Rods contain one type of photosensitive molecule, respond to dim light and are used for night vision; they play little or no role in color vision. Amazingly, experiments have shown that a single photon (elementary particle) of light can activate one rod cell.
Photo K
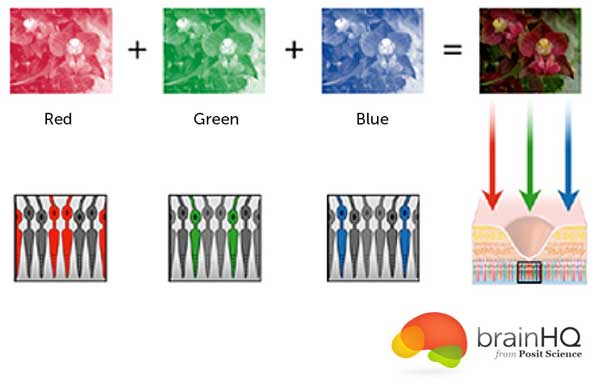
The retina contains about 6 million cone cells that are concentrated in the fovea but decrease in numbers away from the fovea. Cones contain one of three types of photosensitive molecules that vary slightly in configuration: L cones respond to red (long-wave length) light, M cones respond to green (medium-wave length) light and S Cones respond to blue (short-wave length) light. Working together, the three types of cones give us color vision (Photo L). Cones function best in bright light, perceive finer visual details and respond faster to stimuli than rods. The cone-rich fovea is the only area of the retina where 20/20 vision is achievable and is critical for seeing fine detail and color. Truly fascinating fact: recent studies suggest that some women may have a fourth type of cone and perhaps a broader perception of color although future studies are needed to define this phenomenon.
Photo L
Hey now! Don’t get all bleary-eyed on me. Take after Himself here and open up them peepers! There’s more to come!
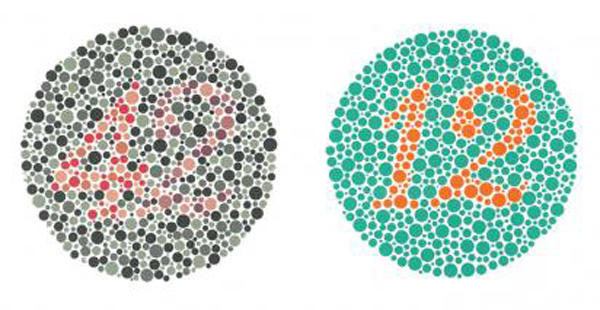
Clinical Correlation #3: As you are aware, some folks are red-green color blind lacking the inability to detect green and/or red colors. About 1 in 50 people, mostly men, lack functioning red- and/or green-sensitive cones, leaving them able to experience only one or two main colors.
Try this: Gaze at Photo M – left image; what do you see? Gaze at Photo M – right image; what do you see? People with normal color vision see a faint number 42 in the left image and the number 12 in the right. People who are red-green color blind cannot see either number.
Photo M
Clinical Correlation #4: Most humans see a wondrous array of colors such as the dishes of powered pigments shown in Photo N. But, some people have achromatopsia meaning they see no color at all and their visual experience consists of different shades of grey ranging from black to white, a bit like images from a black and white TV set (Photo O). Achromatopsia is extremely rare, effecting about one in 33,000 persons.
Photo N
Photo O
Try this: Here’s one last demonstration to compare differences between rods and cones. In 2002, neurobiologist Margaret Livingstone found that the Mona Lisa (Photo P) demonstrates the different processing capabilities of rods and cones. Because da Vinci painted the lips with low-detailed brush strokes, rods perceive this feature better than cones. The eyes were painted with high-detailed brush strokes best perceived by cones. Thus, her test subjects who stared at the mouth, saw the lass as less cheerful than if they focused on her eyes. As Livingstone put it, “She smiles until you look at her mouth, and then it fades, like a dim star that disappears when you look directly at it.” Try it and see if it works for you.
Photo P
Now, time has come to put everything together. Take a deep breath and let’s “see” how normal vision works in three easy steps! Ha, ha.
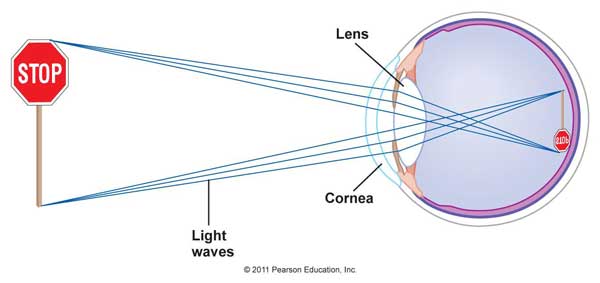
Step #1 – Light from object to retina: think of each eye as a separate camera and imagine looking at a stop sign (Photo Q). Because each eye faces forward and is housed in a different bony orbit, each eye detects a slightly different image of the stop sign. As light rays travel from the stop sign, they strike the corneas and are refracted; then, lenses and humors add further refraction such that the image arrives at the retina upside down and backward (Photo Q). I didn’t mentioned this wee fact before but ‘tis true!
Photo Q
Step #2 – Light activation of rod and cone cells: Light rays from the stop sign pass through the retinal layers (Photo R – box 1) to reach rods and cone cells. Photons strike photosensitive molecules of rod and cone cells (Photo R – box 2) and presto, MAGIC! Just joshing you…. Light rays striking the photosensitive molecules causes them to undergo phototransduction, a complex process wherein light photons are converted into electrical signals that propagate back through the retinal cells to the ganglion cells (Photo R – box 3). Signals reach the ganglion cells and follow their axons to the optic nerve (Photo R – box 4).
Photo R
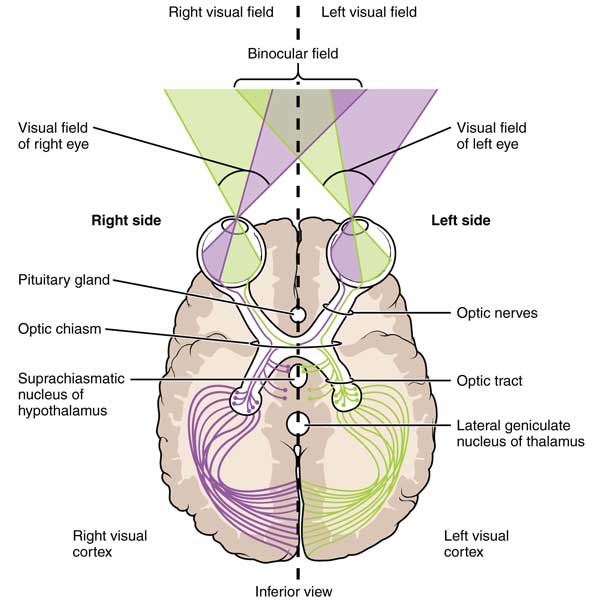
Step #3 – Projection of visual electrical signals to the brain: This step is challenging but stay with me, students! Step three is where everything comes together!
NOTE: Photo S is a schematic of eyes, optic nerves and brain as if seen from a patient’s feet; thus, the subject’s right is on your left! OK, hold on and let’s go!
Retinal signals from the stop sign image follow the optic nerves, each a bundle of about one million axons. Optic nerves form at the back of each eyeball and meet just behind the pituitary gland at the optic chiasm (Photo S). Here nasal retinal nerve fibers cross over such that fibers carrying signals from the right temporal retina (lavender) and the left nasal retina (lavender) project to the right visual cortex (lavender) of the brain; fibers carrying signals from the left temporal retina (green) and the right nasal retina (green) project to the left visual cortex (green). The visual cortices (pl.) are located in right and left occipital lobes of the brain. Crossing over (decussation) of the nasal fibers aids in the integration of visual information. After the chiasm, the optic nerves are renamed optic tracts. Optic tracts have other connections along the way to the visual cortices but these are beyond the scope of this lesson.
Try this: Open fingers of one hand and grip the most projecting part of the back of your skull; this is your occipital bone (from Latin ob, behind, and caput, head). Both occipital lobes lie deep to the occipital bone.
Visual cortices are essential for vision because, here, the stop sign image from each retina is received as electrical signals. Occipital cortices integrate info, recognize form, identify objects, determine location, evaluate spatial cues, detect motion and provide memory. They also augment depth perception where visual fields from both eyes overlap (Photo S – binocular field). The cortices also relay info to other brain sites involved with balance, meaning, etc.
Understand that if vision is normal, all three steps occur in fractions of seconds. Neuroscientists perform numerous studies to discern how the visual cortices work. Simply put, eyeballs collect visual information but we “see” with our brains!
Photo S
Peek to the right…peek to the left…do you see what I seeee?
Possible Spoiler Alert: Speaking of depth perception, our genius author, Diana, writes about binocular vision in her 5th book, The Fiery Cross: here our beloved Claire treats another patient:
“You don’t have any binocular vision,” I said… He looked down into the palm of his hand, closing one eye, then the other, as though some answer might be found among the lines there. “Your eyes are fine,” I assured him. “It’s just that they don’t work together… for one reason or another, the brain never learns to merge the images coming in from both eyes in order to make a three-dimensional image.”
The ability to see in three dimensions is called depth perception, binocular vision or stereoscopic vision. Claire (Diana, snort!) is absolutely correct; if the eyes (and extraocular muscles) are otherwise normal, the ability to see in 3-D occurs in the brain. Recall that each eye collects a slightly different version of an object because our eyes face forward and each lies in a different bony orbit (if our eyes were on the sides of our heads we would not enjoy depth perception). The visual data from the two slightly different images are sent to visual centers of the occipital lobes and there is integrated into a single 3-D image. Our amazing brain does this instantaneously without conscious direction!
Try this: Photo T is a pair of stereoscopic photos of the moon. With your face about 10 cm / 16 inches from the screen, widen your eyes slightly. Now, gently start to cross your eyes until the moons fuse into a 3-D moon in the center. If you can perceive the depths of the moon’s cratered surface, this is was done by your remarkable brain! Did it work? If not, try the next image.
Photo T
This is a pair of stereoscopic images of Machu Picchu each overlain with a red diamond and an outline of the hand (Photo U). Gaze at the two images using the screen distance mentioned above. Gently cross eyes until the two diamonds fuse into one central 3-D diamond. See the city with mountains behind it? Grand!
Photo U
Some students have asked for explanations of nearsightedness and farsightedness so let’s finish the lesson with these topics. The following are simplistic explanations because optical science is detailed.
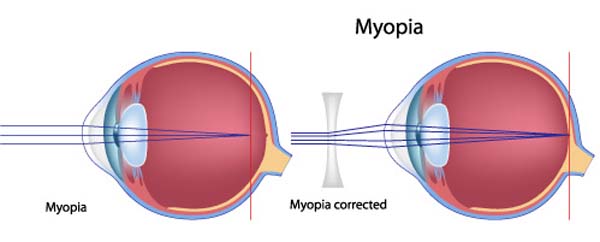
Myopia, also known as being nearsighted (US) or short-sighted (Britain), is a condition wherein light entering the eyeball focuses in front of the retina rather than directly on it (Photo V – left image). Close objects appear in focus but distant objects are blurry. In most instances, myopia is caused by an elongated eyeball or a steep corneal curvature and the eye’s lens cannot correct the problem. Nearsightedness can be treated with eyeglasses, contact lenses or refractive surgery.
Myopia can be corrected using a diverging lens that spreads light rays from distant objects bringing them to focus on the retina (Photo V – right image). An eye specialist determines the correct lens for myopia using optical measurements of the eye.
Photo V
This is a startling statistic: twenty-five percent of the world’s population is nearsighted and the rate is increasing (Photo W)! Evidence suggests that indoor living, close work (e.g. computers), and inside play are contributing factors. A recent Chinese study showed that children who played outdoors 40 minutes longer per day than a control group had a 23% reduced likelihood of developing myopia (JAMA, Sept. 15, 2015). Reminder of the adage, “use it or lose it!”
Photo W
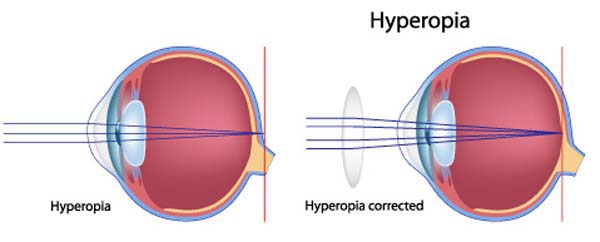
Hyperopia, also known as farsightedness (US) or long-sightedness (Britain) is a condition wherein light entering the eyeball focuses behind the retina rather than directly on it (Photo X – left image): close objects appear blurry but distant objects are in focus. In most instances, the eyeball is too short or the cornea is too flat and the eye’s lens cannot correct the problem. Farsightedness can be treated with eyeglasses, contact lenses or a lens implant.
Hyperopia can be corrected using a converging lens that bends light rays from near objects to focus on the retina (Photo X – right image). Again, an eye specialist determines the correct lens for hyperopia using optical measurements of the eye.
Photo X
Okay, students, the bell just rang and this lesson is over. But, let’s not leave without at least one more glimpse of Jamie! Okay, how about two? Mmphm…..as ye ken, Starz episodes contain a plethora of subtleties that are spied using our astute and wonderful vision.
Here’s a good example: do ye ken the scene wherein Jamie flips Dougal the middle finger? In western cultures giving someone the finger or flipping someone “the bird” communicates extreme contempt. Oh, you dinna believe Jamie did that to Dougal? Well, look closely (Starz, episode 102, Castle Leoch): remember when Jamie takes a beating for Longhair and her loose ways? He bows to Colum and then glares at his uncle Dougal. Yep, that’s the one!
That beating was administered by Rupert but was orchestrated by the masterfully manipulative Maestro Dougal. See Jamie’s shrewd subtle show of utter contempt for his black-booted uncle? Here, this one’s for you, big bad-ass brother of my mother! Hee hee!
That’s it! Hope you have enjoyed our last five anatomy lessons on the amazing, astounding, astonishing eye. Much more is known about the molecular biology and neurochemistry of vision but it is too detailed for our lessons. Let’s be grateful for our vision that is so easily taken for granted!
The Eyes Have It!
Now, let’s get this straight,
The eyes are just great,
As they bring our world into view!
Crisp vision’s a trait
That we shouldn’t berate,
Seeing clearly gives us a clue.
Please don’t agitate,
If a lens is your fate,
Not worth getting into a stew.
Let’s all celebrate,
The eyes are a gate,
Into the wonderful soul that is you!
A deeply grateful,
Outlander Anatomist
Photo creds: Starz, www.boundless.com (Photo E), www.brainhq.com (Photo L), www.colourblindawareness.org (Photos N, O), www.commons.wikimedia.org (Photo S), www.studydroid.com (Photo D), www.digital-photography-tips.net (Photo U), www.en.wikipedia.org (Photos A, F, G), www.faculty.virginia.edu (Photo J, by Benjamin Cummings), www.hobart.com (Photos P, V), www.kaiserscience.wordpress.com (Photo Q), www.livingwelldementia.org (Photo K), www.mikenudleman.com (Photo T), www.myeyes.com (Photo X), www.peoi.org/Courses (Photos H, M, P), www.healthisright.com (Photo C), www.seekingalpha.com (Photo W), www.studyblue.com (Photo B), www.vi.cl (Photo R), www.webvision.med.utah.edu (Photo I)













This was a very convenient lesson. I’m probably going to have cataract removal surgery in the near future, but first I have to have a Retinal Consult. The ophthalmologist was concerned because my retina seems to be thin, and she doesn’t want to damage it during the cataract removal. By the way, I am an extremely near-sighted 71 year-old. The next few weeks should be interesting. Thank you for your time in bringing these lessons, and great pictures, to us.
Cheryl, sending good thoughts your way. Now days, cataract surgery has become almost routine but there are always extenuating circumstances. Sounds like an excellent idea to check with a retinal specialist to determine if you are a good candidate for the surgery. Best of luck!