Anatomy Def: Jocasta’s Blindness – painful pressure in the eye
Outlander Def: Jocasta’s Joy – pain relieved by smoking hemp flowers
Greetings, anatomy students!
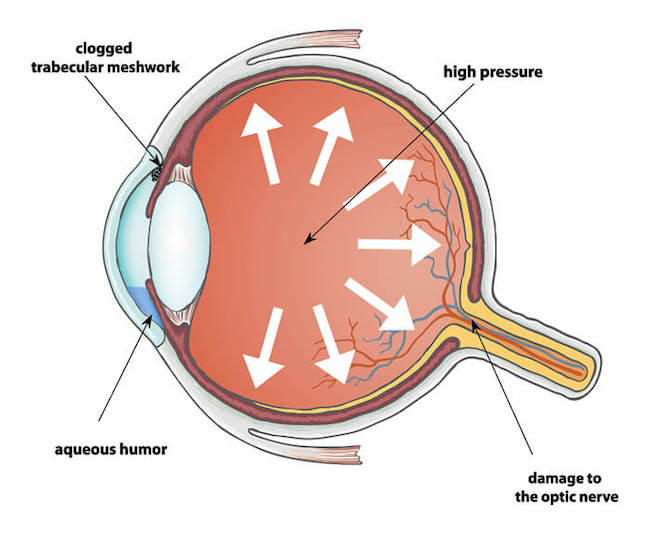
Let’s learn about the disease that robbed Jocasta Cameron of her eyesight: Glaucoma. Yep, that’s the one. Glaucoma (glaw-koh-muh), is a word derived from the Greek glaukommatos meaning “gray-eyed.”
But, first, a wee divergence for a quick anatomy lesson of the eye which, in my opinion, is the body’s most anatomically elegant structure. This brief review is necessary to glean any useful understanding about this disease.
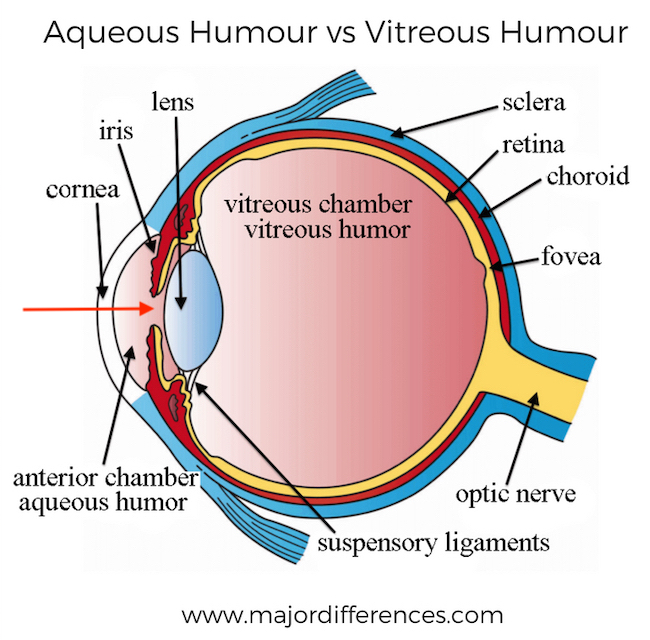
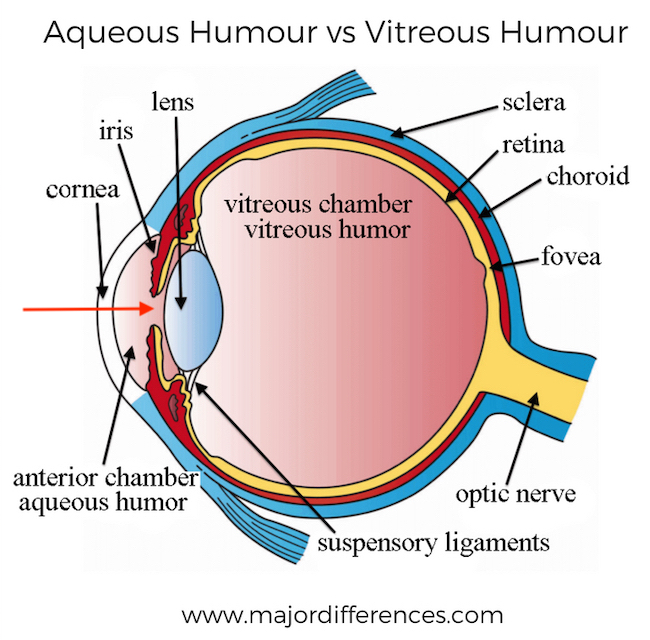
Eyeball: The next image shows a horizontal-section of the right eyeball (globe) as seen from above. The diagram shows in succession (from L to R) the cornea, iris, and lens; the opening in the middle of the iris is the pupil (red arrow).
Two Chambers: The eyeball contains two important spaces (peachy-pink in the image, below). A large area behind the lens is the vitreous chamber – it is shaped like a sphere. In front of the lens is the smaller anterior chamber – it is shaped like a disc. The pupil supplies an open route between the two spaces.
Optic Nerve: At the back of the globe is the large optic nerve, an extension of the brain into the the eyeball. It is formed by filaments from cells of the retina. When photons (packets) of light excite retinal cells, they send signals via the optic nerve to the brain where it interprets the signals as the object viewed.
Vitreous Chamber: The vitreous chamber is filled with the vitreous body, a jelly-like material that becomes more fluid with age.
Anterior Chamber: The anterior chamber is filled with a watery substance known as aqueous humor.
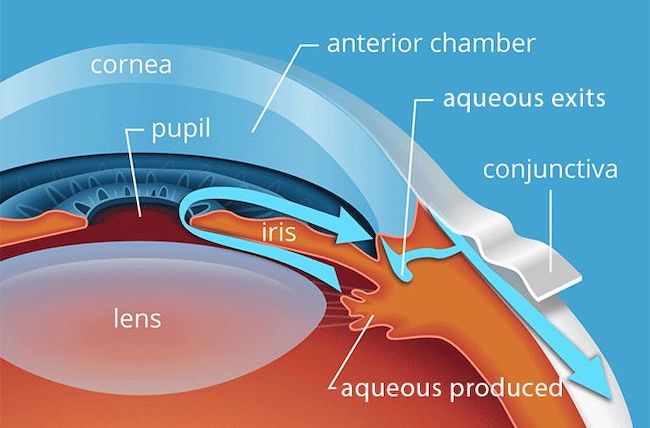
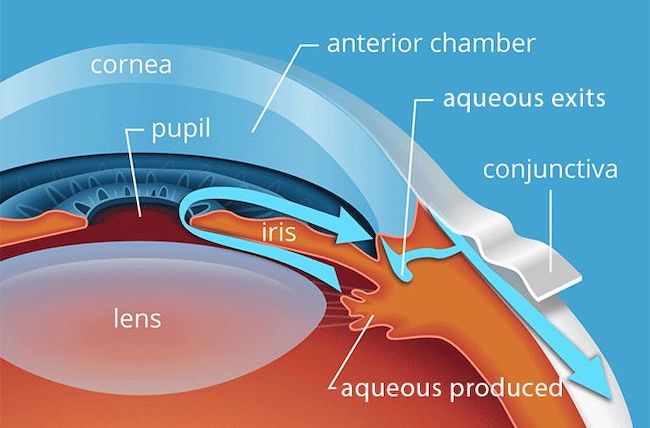
Aqueous Humor: Aqueous humor is similar to blood plasma; it fills the anterior chamber (next image). Aqueous humor is produced 24 x 7 – continuously made by tissues near the lens and constantly drained by tissues near the iris.
Blue arrows show the direction of flow of the aqueous humor from its production site, through the pupil into the anterior chamber, and then into nearby exits to be carried away.
A very quick lesson, indeed!
Learn more about the eye in not one, but five anatomy lessons!
Q: Why so many lessons, prof?
A: Because the eye is exceedingly complex! 🤓
The lessons are:
*Anatomy Lesson #29: The Eyes Have It!
*Anatomy Lesson #30: Aye, Eye, The Eyes!
*Anatomy Lesson #31: An Aye for an Eye!
*Anatomy Lesson #32: A Real Eye Opener!
*Anatomy Lesson #33: Eyemax!
Glaucoma: When a person suffers from glaucoma, aqueous humor is either overproduced or the production is normal but it does not drain properly, or both may be culprits. If the fluid cannot drain, not only does it fill the anterior chamber, it also backs into the vitreous chamber.
Symptoms: So, what happens when aqueous humor builds up? Well, several things, usually over time.
-
- Eye pain or pressure
- Headaches
- Rainbow-colored halos around lights
- Nausea and vomiting
- Red eyes
- Loss of side (peripheral) vision
- Low vision, blurred vision, narrowed vision (tunnel vision)
- Blind spots
- Blindness
- Not-So-Fun-Fact: Glaucoma is the leading cause of blindness in people over 60.
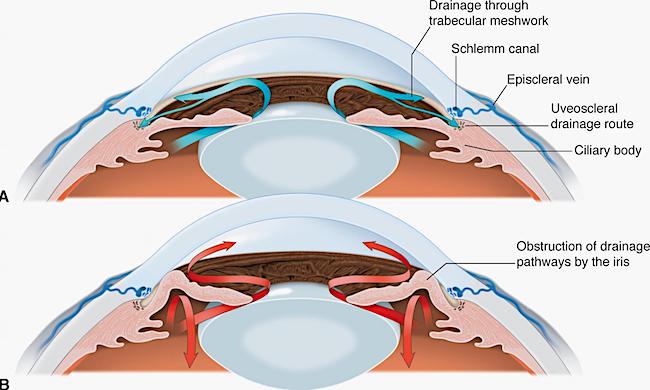
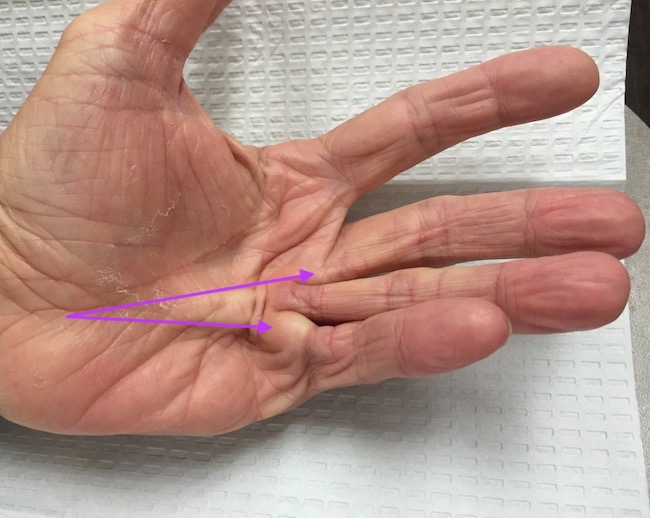
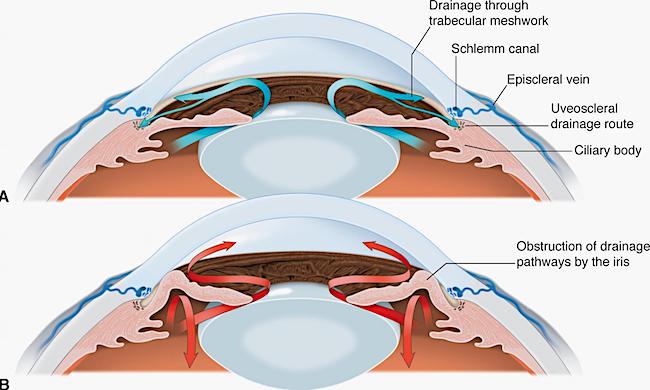
Comparison: Let’s compare a normal eye (panel A) with a glaucomatous eye (Panel B) so we understand how things work.
-
- Panel A shows normal flow and removal of aqueous humor
- Panel B shows aqueous humor accumulating in anterior chamber and in vitreous chamber because there is too much or it does not drain properly.
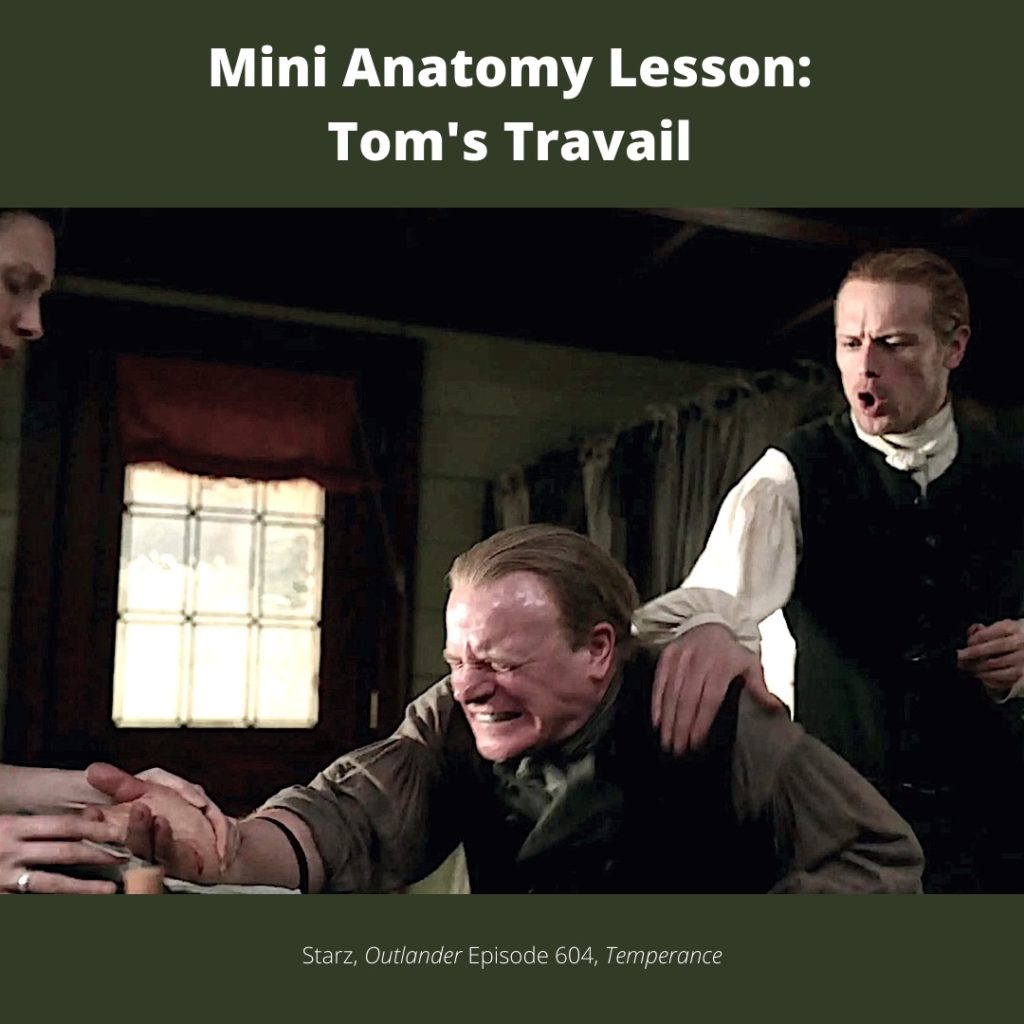
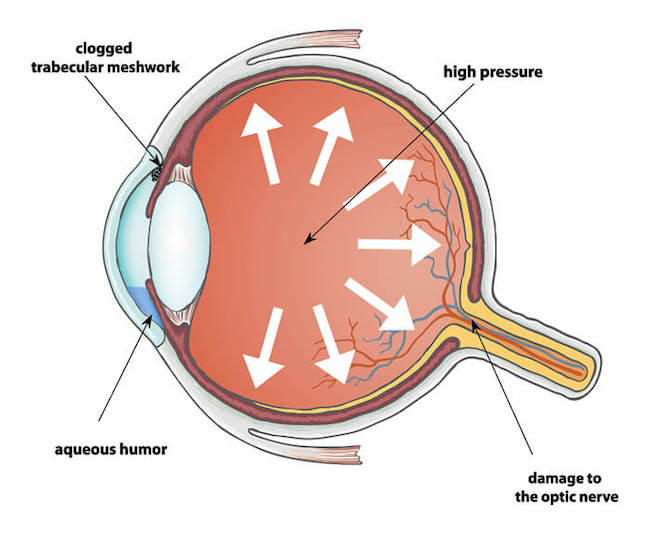
Jocasta: Now, we come to the root of Jocasta’s problem (next image). As intraocular pressure builds because of too much aqueous humor, it presses against the fragile retina (yellow layer) and optic nerve causing irreversible damage. This means the normal response of the retina to photons of light and subsequent transmission to the brain are diminished or cease altogether. Such changes are typically accompanied by misery and pain.
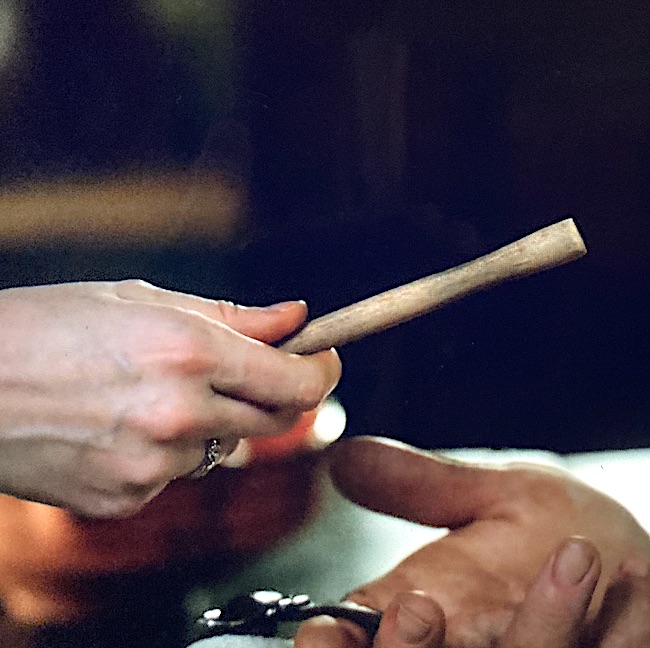
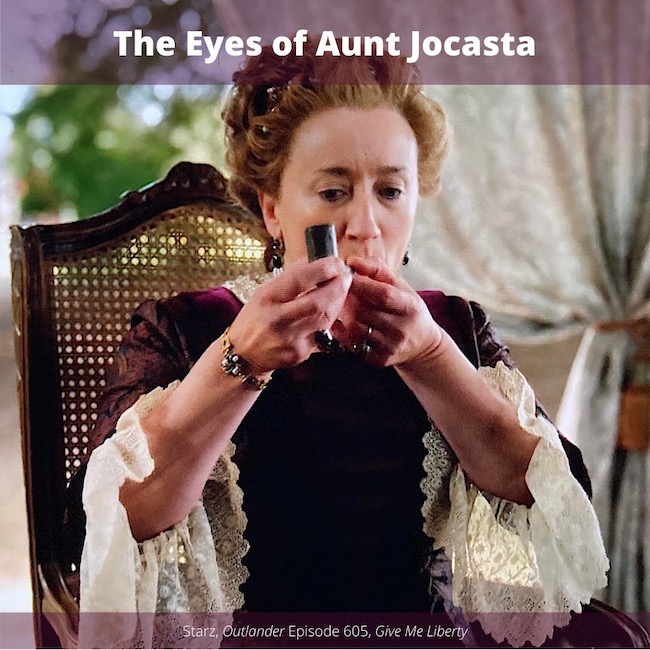
Unfortunately, Claire lacks current methods and medicaments to treat glaucoma. She can provide, however, hemp flowers for a wee pipe!
Now, does this really work?
Yes. Yes. It does.
Smoking hemp decreases intraocular pressure, thus relieving the pain and discomfort of pressure against retina and optic nerve.
Note: Hemp also reduces blood pressure throughout the entire body, a side effect which might not be beneficial to all individuals, depending on their general health.
But, our Auntie Jo feels better and is even giddy!
(I love those goblets! 😍)

I should clarify that research showing the effects of smoking hemp on glaucoma wasn’t proven until the 1970s, a few years after Claire’s return to the eighteenth century. In her defense, the good doctor may have learned anecdotally about such benefits before she took her long and winding road back to Jamie.
Etiology (cause) of Glaucoma: Although we speak of glaucoma as a single disease, it is not. Glaucoma is a group of eye diseases that cause vision loss and blindness. The two most common types are:
-
- Open angle – drainage routes are blocked – progresses slowly
- Closed angle – drainage routes are blocked – progresses more rapidly and is usually more severe
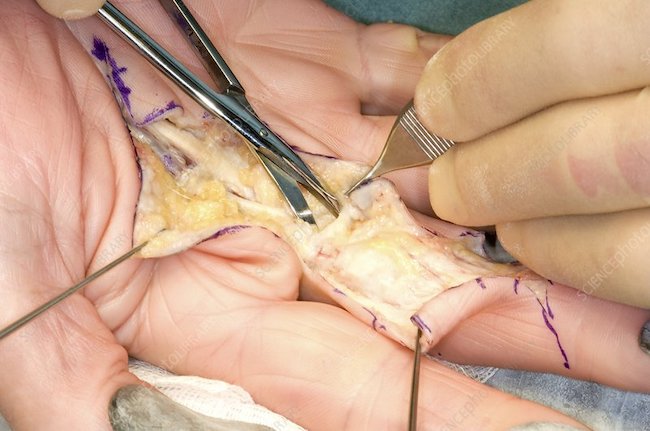
Treatments: Treatments include eye drops and surgery. These may be used separately or together for treatment.
-
- Eye drops – reduce intraocular pressure. Glaucoma must be detected early to be effective
- Laser Eye Surgery – Improves drainage via normal routes
- Tube Shunt Surgery – Small device is placed in eye to augment fluid drainage
- Trabeculectomy – Delicate surgery creating new drainage ports
Claire’s solution of hemp smoking is entirely different than what she does in the book. Read on and you will see why.
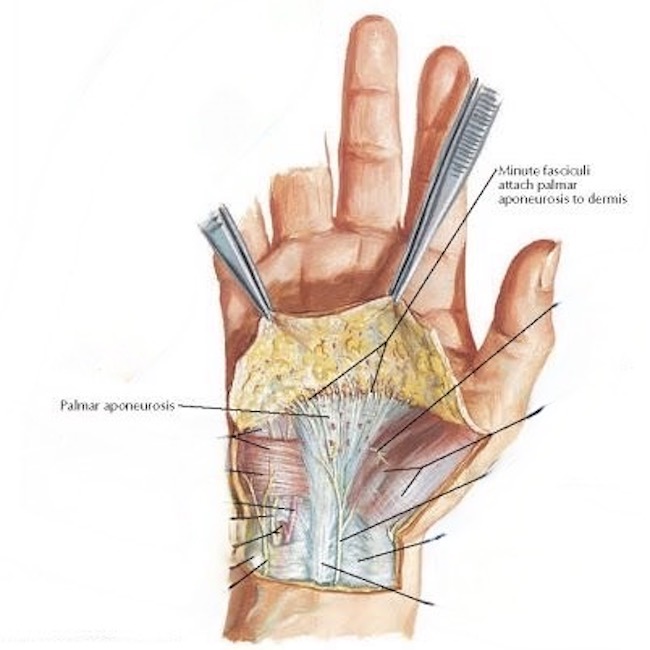
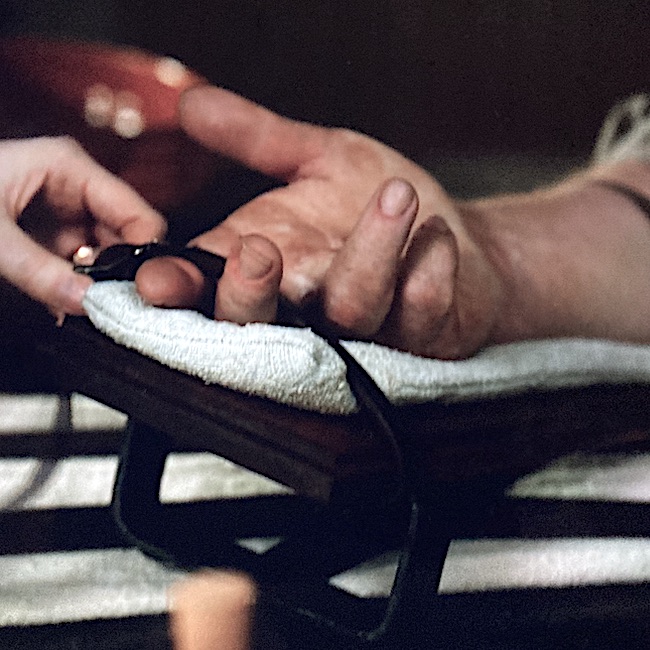
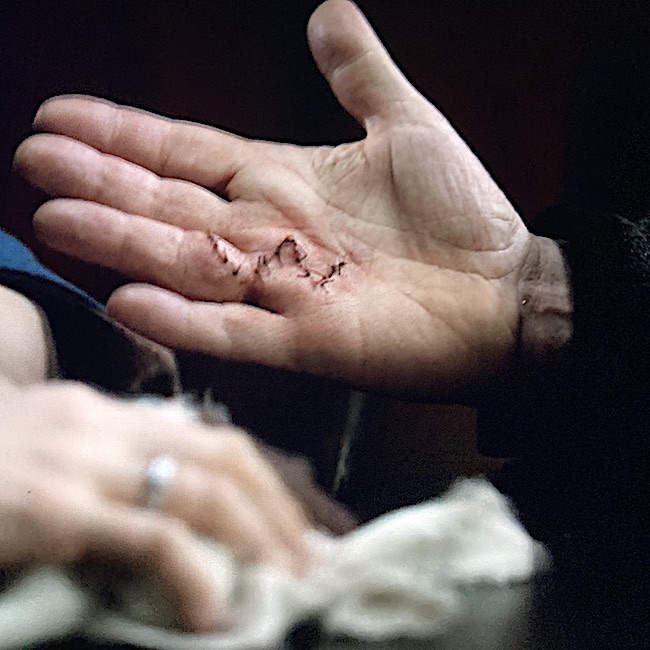
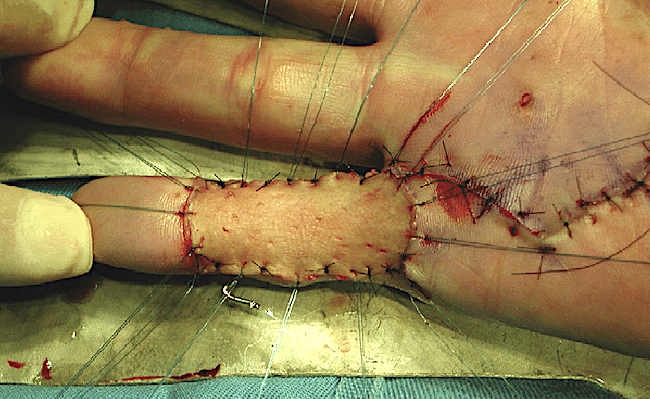
Read about Claire’s gutsy and unorthodox treatment of Jocasta’s glaucoma in Diana’s sixth big book, A Breath of Snow and Ashes. Here, she pierces the eyeball with a carpet needle, allowing excess fluid to seep out and relieve the unrelenting pressure and pain.
(Pssst….. The escaping fluid is aqueous humor, not vitreous 🤫)
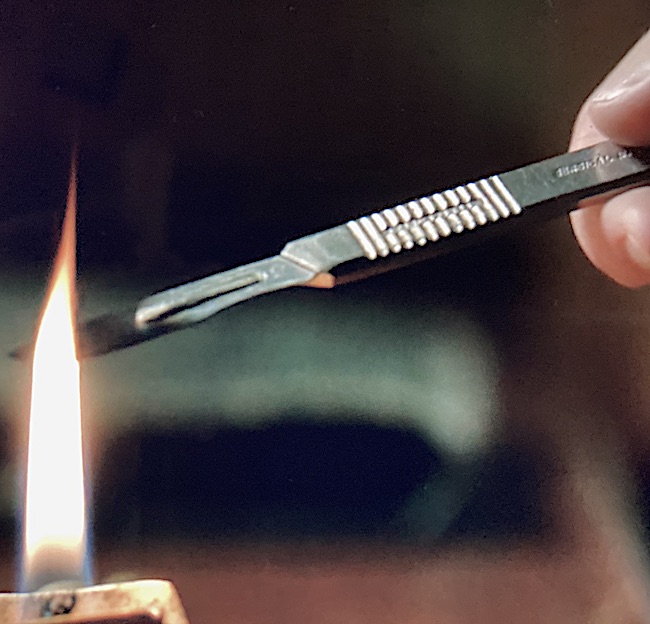
Even as I talked, I’d got out the tiny spirit lamp I carried in my case. The fire had been allowed to burn down on the hearth, but there were still live coals; I bent and lit the wick, then opened the needle case I’d taken from the sitting room and abstracted the largest needle in it, a three-inch length of steel, used for mending carpets.
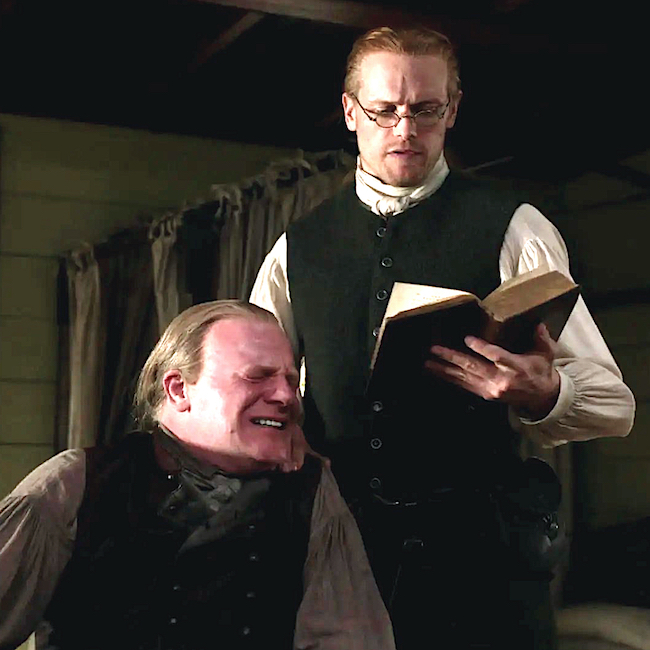
“You aren’t …” Jamie began, then broke off, swallowing.
“I have to,” I said briefly. “There’s nothing else. Hold her hands.”
He was nearly as pale as Jocasta, but he nodded and took hold of the clutching fingers, pulling her hands gently away from her head.
I lifted away the linen bandage. The left eye bulged noticeably beneath its lid, vividly bloodshot. Tears welled up round it and overflowed in a constant stream. I could feel the pressure inside the eyeball, even without touching it, and clenched my teeth in revulsion.
No help for it. With a quick prayer to Saint Clare—who was, after all, patroness of sore eyes, as well as my own patron saint—I ran the needle through the flame of the lamp, poured pure alcohol onto a rag, and wiped the soot from the needle.
Swallowing a sudden excess of saliva, I spread the eyelids of the affected eye apart with one hand, commended my soul to God, and shoved the needle hard into the sclera of the eye, near the edge of the iris.
… I withdrew the needle carefully, though as fast as I could. Jocasta had stiffened abruptly, frozen stiff, hands clawed over Jamie’s. She didn’t move at all, but made small, shocked panting sounds, as though afraid to move enough even to breathe.
There was a trickle of fluid from the eye, vitreous humor, faintly cloudy, just thick enough to be distinguishable as it flowed sluggishly across the wet surface of the sclera. I was still holding the eyelids apart; I plucked a rag from the goldenseal tea with my free hand, squeezed out the excess liquid, careless of where it went, and touched it gently to her face. Jocasta gasped at the touch of the warmth on her skin, pulled her hands free, and grasped at it.
I let go then, and allowed her to seize the warm rag, pressing it against her closed left eye, the heat of it some relief.
Now, you might think this extreme, but the only other remedy Claire could offer would be to remove one or both of Jo’s eyes!
Well done, Claire! 👏🏻👏🏻👏🏻
See Claire treat Auntie’s glaucoma in Outlander episode 605, Give Me Liberty!
I think Aunt Jo might welcome the hemp just a wee bit more than that needle jab, eye? 😉
The deeply grateful,
Outlander Anatomist
Follow me on:
Photo Credits: Starz, www.aao.org, www.allaboutvision.com, www.majordifferences.com, www.ohioeyesurgeons.com, www.2020pittsburgh.com