Anatomy Def: The belly wall is known by anatomists as the anterolateral abdominal wall (why use a simple word when a complex one will do?). 😉
Outlander Def: Claire’s Despair – Malva’s Mutilation! 😱
Before we begin this lesson, I have a true story to share…. In 2016, I asked Diana Gabaldon if nominative determinism was involved in her choice of Malva’s name because “mal” is the Latin word root meaning “evil” or “bad,” which clearly could apply here.
Why did I ask this? Think about it…. There’s mal-ware, mal-nutrition, mal-adapted, mal-content, mal-practice, mal-evolent, mal-odorous, and Mal-va! 😳
Diana answered, “No, I got it off a bottle of black malva shampoo!”
Haha. Love it! 😜
OK, anatomy students, let’s get on with our lesson.
Warning: The following images detail the final events of episode 606, “The World Turned Upside Down.” If you couldn’t watch this part of the episode, you might not want to read this lesson!
Recap: Claire was in her surgery under the influence while someone “stomped through the nasties” with Malva.
Never dreaming her beloved garden would be the site of a massacre, Claire spies Malva’s lifeless body, throat thoroughly mangled! 😯

Realizing her infant may still be alive, Claire springs into action, slicing open Malva’s gown with her garden knife.

Moving with speed and surety, Claire slices Malva’s belly wall vertically and to the left of her navel, a vertical cesarean section.
Claire works ruthlessly with such intent and determination that Malva’s lifeless body shutters from her efforts.

Claire releases the infant from the womb and realizing its life is fleeting. She performs mouth to mouth resuscitation and chest compression using two fingers. But, alas, her efforts fail.

Goodness, this is hard to review, even using still images.
After this episode was over, my husband, who is not a book reader, turned to me and asked, “Is that in the book?” ‘Yes,” I answered. He remarked, “That is going to be hard to explain.”
He then added, “ Now, they have to figure out who murdered Malva.
”Who do you think it might be,” I asked.
“Well, I would look to the brother, first,” he said.
Amazed, I asked “Why?”
His answer: “Because in patriarchal systems, male relatives often kill women who bring shame upon their families.” (See footnote at end of lesson) 😲
‘Nuff said!
With this horrific scene as backdrop, let’s talk anatomy of the belly wall.
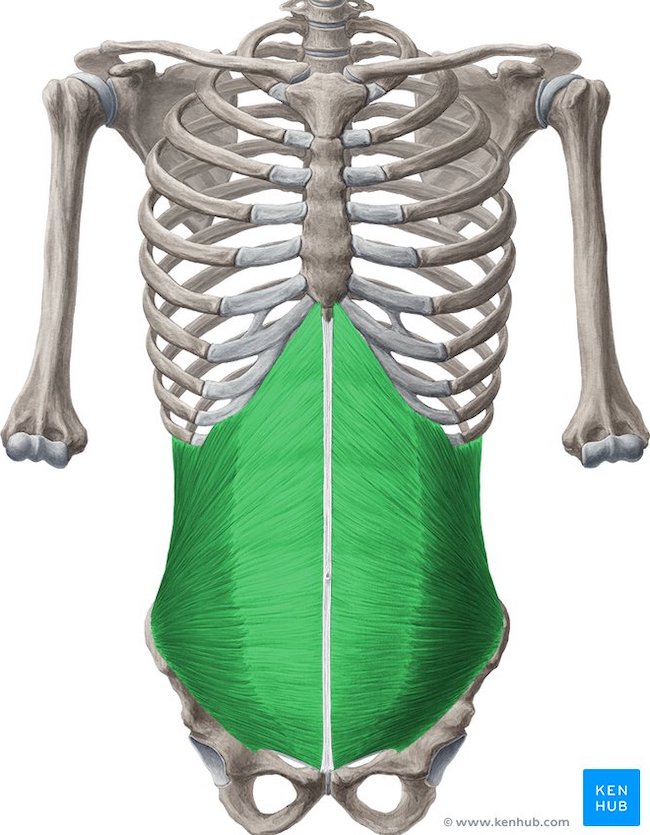
Abdominal Wall: The abdominal wall is a cylindrical region of the body bounded above by costal cartilages, ribs, and sternum (xiphoid) and below by iliac and pubic bones (green area in image below).
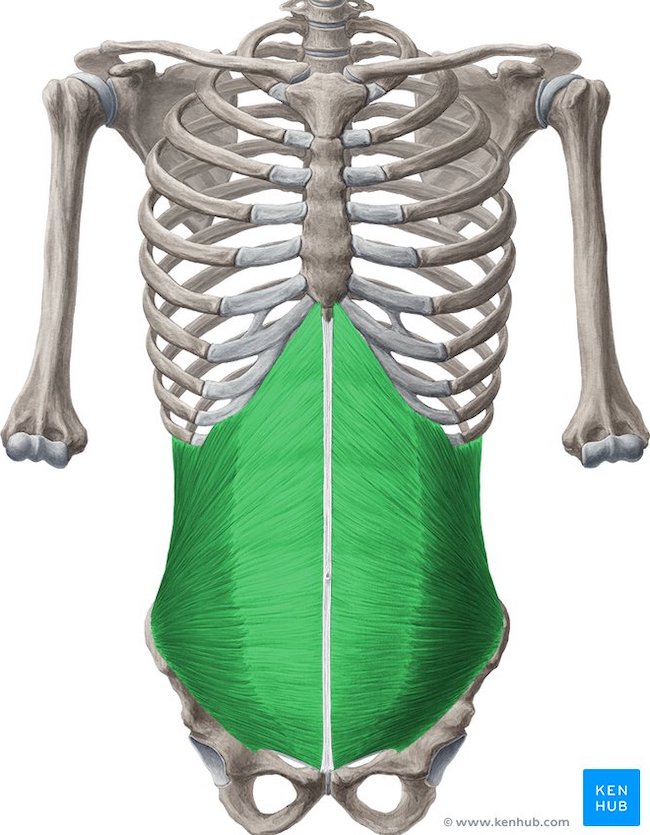
Anatomists typically divide the abdominal wall into anterolateral and posterior parts. The term, anterolateral, means the front (antero-) and sides (-lateral) of the wall. The term, posterior, refers to the back of the wall.
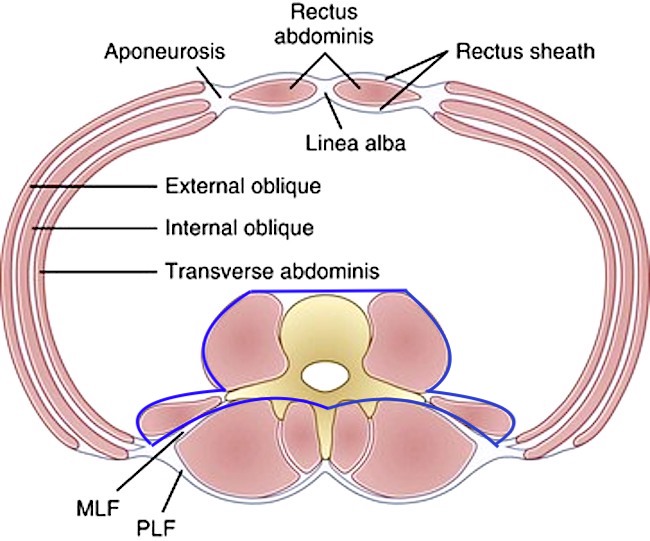
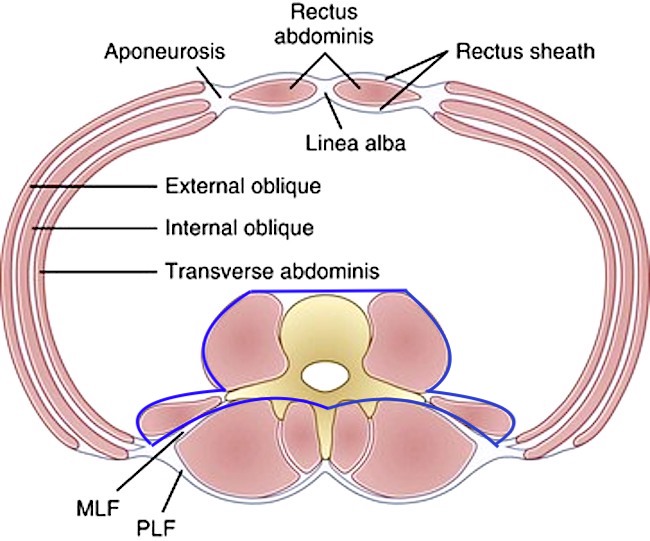
These regions are best demonstrated in a cross-section (horizontal) through the torso.
The figure below shows the two regions. The area bound by blue lines is the posterior abdominal wall. The remainder of the large pink oval is the anterolateral abdominal wall. (Psst….Dinna fret about all the names. Will explain below).
Anterolateral Abdominal Wall (AAW): Succinctly put, the anterolateral abdominal wall is the flexible and expandable part…. a.k.a., the belly. The posterior abdominal wall has limited flexibility and is unable to expand to any significant degree.
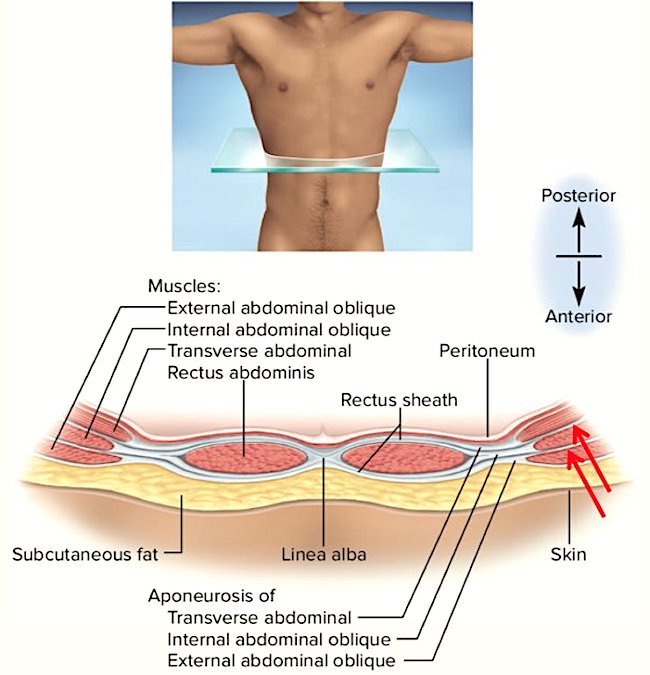
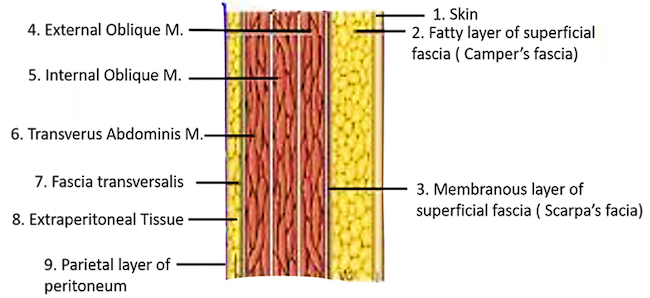
The main reason the AAW can expand is because it is made of soft tissue layers (no bones). The layers vary depending on the site. The following image is a cross-section of the AAW above the navel.
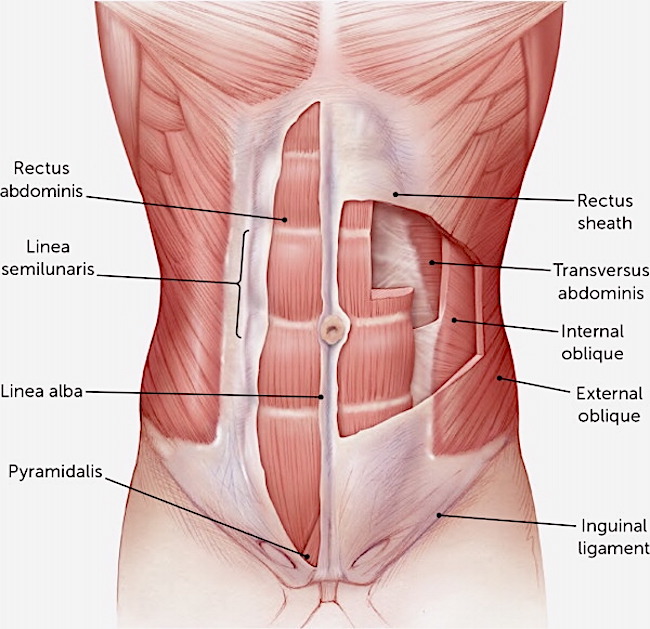
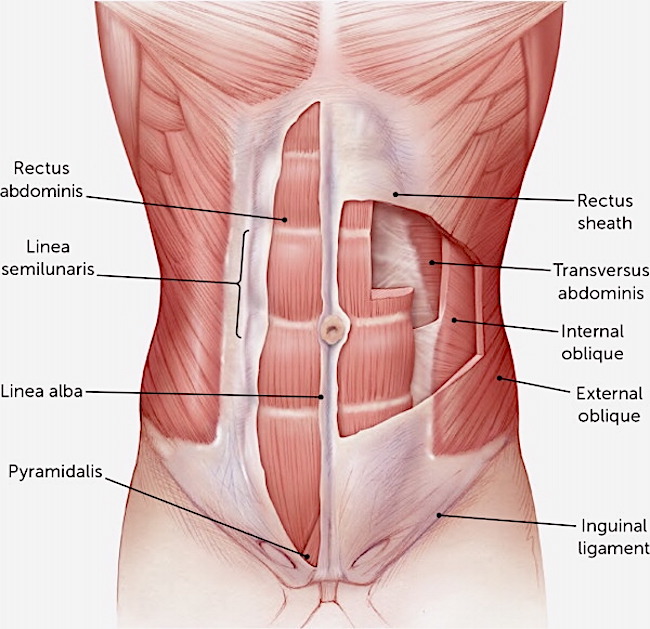
The central area marked as linea alba is a vertical line of connective tissue that unites right and left halves of the AAW. It is a nearly bloodless line and therefore can be cut with little blood loss.
On either side of the linea alba are right and left rectus abdominis muscles. These run vertically.
Using the image below, at the sides of the AAW, three layers of muscle appear, from outer to inner:
-
- external abdominal oblique (EAO)
- internal abdominal oblique (IAO)
- transversus abdominis (TA).
The following image shows the muscle pattern from a frontal (anterior) view. Note the linea alba. Clearly, the belly wall enjoys a good deal of muscular support.
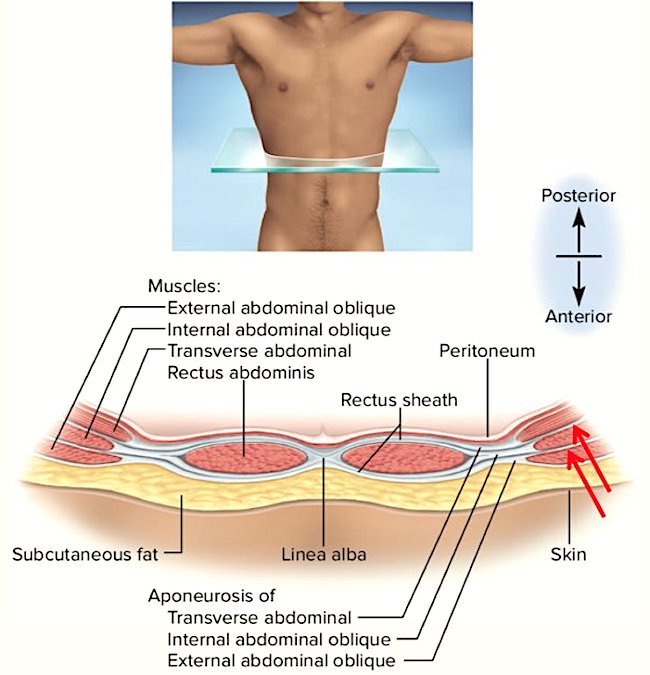
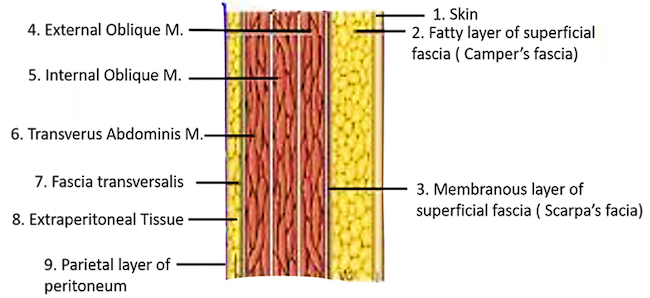
So, how thick is the AAW? Well, that depends on the individual. Moving to the next image, a magnified cross-section through the AAW, we find that the lateral AAW is composed of nine layers (three are muscle layers)!
-
- Skin
- Fat layer (we accumulate varying amounts of fat in this layer)
- Superficial fascia
- EAO
- IAO
- TA
- Transversalis fascia (connective tissue)
- Extraperitoneal layer (more fat and connective tissue)
- Peritoneum (membrane lining abdominal cavity
Nearer the midline, AAW is composed of seven layers because it has only one muscle layer, the rectus abdominis.
Either way, that is a LOT of layers!
Functions of the AAW: You might ask why is this part of the body designed to be flexible and expandable? Here are some reasons:
-
- Maintains upright position
- Moves the trunk (rotation, flexion, extension, bending sideways)
- Protects abdominal viscera
- Absorbs shock (remember BJR punching Claire in stomach in ep 106?)
- Supports pregnancy
- Increases intra-abdominal pressure (coughing, vomiting, childbirth, sneezing, defecation)
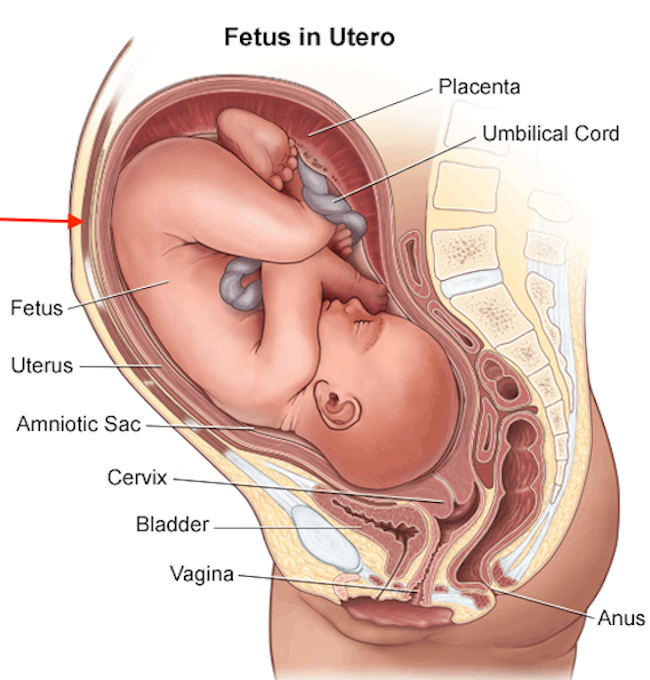
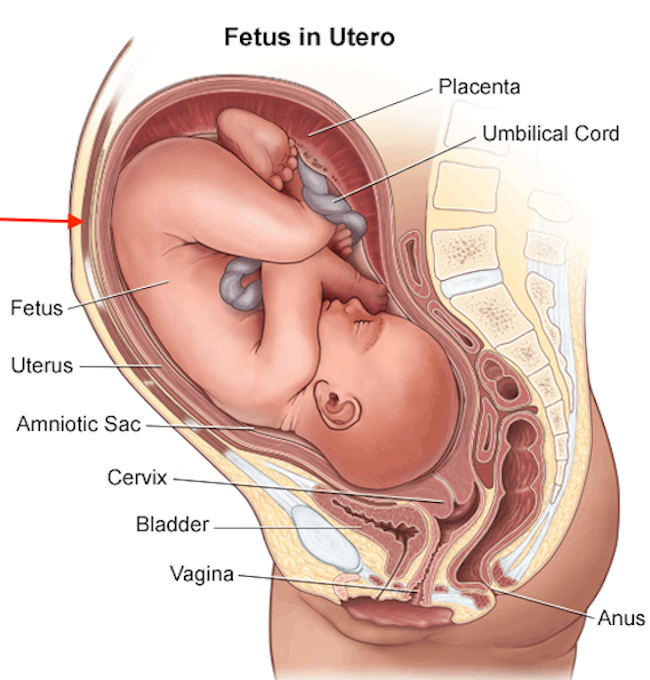
It is a darn good thing the AAW is flexible, especially for a pregnant woman. The next image shows a fetus during the third trimester. The uterine wall is labelled. The red arrow indicates the muscle layer of the AAW.
It as well as the other layers expand dramatically over the course of a pregnancy. The relatively slow growth of the fetus allows the belly wall to accommodate to the stretching, usually without tears, although these do occur (hernia). This image is close to Malva’s condition when she was murdered.
So, there we have it in a nutshell, albeit a rather large one. We need an intact AAW to function well in our lives as it serves multiple purposes.
Learn more about the AAW in Anatomy Lesson #16, “The Abdomen.” There is much more to learn about this part of our anatomy – Lesson #16 explores this in greater depth.
NOTE: The AAW is essentially the same in females and males except the groin region, there we find differences. Lesson #16 explains these.
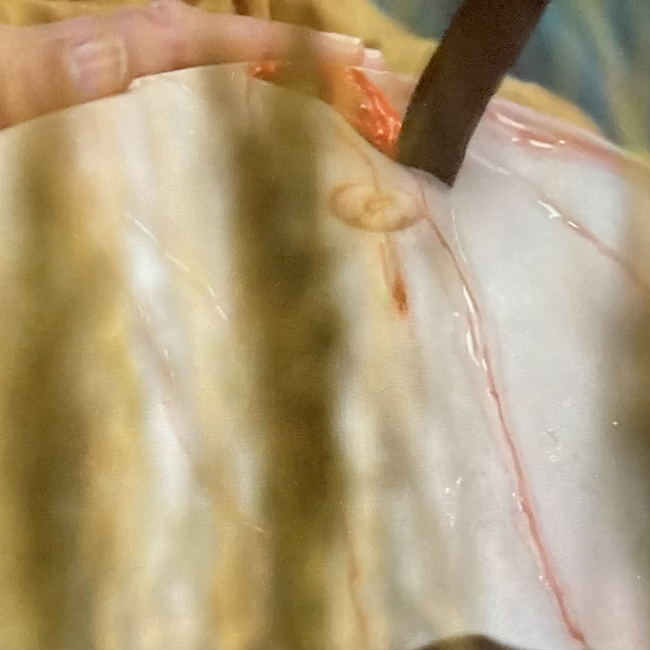
FX: Now, how well did Starz FX do with Outlander 606? Pretty darn good if you ask me. Here are some examples:
-
- As Claire begins her cut, there is a small stream of blood-tinged fluid which is consistent with the location of the cut, that is, very near the linea alba (see above). There would be little blood flow at this point as the cut is only through the belly wall.
- Malva’s navel does not look realistic because it appears largely normal. In late pregnancy, it usually pooches outwards due to increased intra-abdominal pressure.
- The pink tissue underlying the skin is fat. It is a bit thick for Malva who is a trim young woman.
- After Claire’s knife pierces the uterine wall and she removes the infant, the C-section now appears dark red because the uterus receives a huge blood supply during pregnancy. Well done.
- Malva’s infant is covered with blood-tinged material, the vernix, a waxy coating to protect the infant’s skin. Yay!
- Malva’s belly is slightly concave after the infant was removed. Horrible, but accurate.
- Mouth-to-mouth on such a tiny person should be done with less force than Claire used – third trimester lung volume is calculated at less than 2 tablespoons per lung! This can accommodate a very tiny amount of air.
- Claire doing two finger chest compression to stimulate the heart is spot on.
Yay, Outlander! Kudos to the FX folks! 
Read about Claire’s emergency C-section in Diana’s sixth big book, “A Breath of Snow and Ashes!”
I smelled the blood and saw her in the same instant. She was lying in the salad bed, her skirt flown out like some gigantic, rusty flower blooming amid the young lettuces.
I was kneeling by her, with no memory of reaching her, and the flesh of her arm was warm when I grasped her wrist—such small, fragile bones—but slack, there was no pulse—Of course not, said the cold small watcher inside, her throat is cut, there’s blood everywhere, but you can see the artery isn’t pumping; she’s dead.
Malva’s gray eyes were open, blank with surprise, and her cap had fallen off. I clutched her wrist harder, as though I must be able to find the buried pulse, to find some trace of life … and did. The bulge of her belly moved, very slightly, and I dropped the flaccid arm at once and seized my knife, scrabbling for the hem of her skirt.
I acted without thought, without fear, without doubt—there wasn’t anything but the knife and the pressure, the flesh parting and the faint possibility, the panic of absolute need…
I slit the belly from navel to pubis, pushing hard through slack muscle, nicked the womb but no matter, cut quick but careful through the wall of the womb, dropped the knife, and thrust my hands into the depths of Malva Christie, still blood-warm, and seized the child, cupping, turning, wrenching hard in my frenzy to pull it free, bring it out from sure death, bring it into the air, help it breathe.… Malva’s body flopped and heaved as I jerked, limp limbs flailing with the force of my yanking.
It came free with the suddenness of birth, and I was swiping blood and mucus from the tiny sealed face, blowing into its lungs, gently, gently, you have to blow gently, the alveoli of the lungs are like cobwebs, so small, compressing its chest, no more than a hand’s span, two fingers pressing, no more, and felt the tiny spring of it, delicate as a watch spring, felt the movement, small squirms, a faint instinctive struggling—and felt it fade, that flicker, that tiny spark of life, cried out in anguish and clutched the tiny, doll-like body to my breast, still warm, still warm.
“Don’t go,” I said, “don’t go, don’t go, please don’t go.” But the vibrancy faded, a small blue glow that seemed to light the palms of my hands for an instant, then dwindle like a candle flame, to the coal of a smoldering wick, to the faintest trace of brightness—then everything was dark.
I was still sitting in the brilliant sun, crying and blood-soaked, the body of the little boy in my lap, the butchered corpse of my Malva beside me, when they found me.
Puir Claire! Puir Malva! Puir wee one!
See Claire as she realizes that all is lost. Mother and child are gone – grief, loss, and futility grip the Good Doctor.
The deeply grateful,
Outlander Anatomist
Follow me on:
Photo Credits: Starz; www.aafp.org; www.anatomyqa.com; www.kenhub.com; www.musculoskeletalkey.com; www.quora.com; www.stanfordchildrens.org
Footnote: In 2017, the United Nations Office on Drugs and Crime reported 87,000 killings of women worldwide – 58% were killed by family members or intimate partners! Alarming stats!