WARNING, all anatomy students! Due to some images, this lesson is NSFW. I must confess a bit of trepidation about this topic not only because it is huge but, because it is also ripe for abuse. Hopefully, you will receive this lesson as a public service, as intended. An equal opportunity professor, the anatomy of both male and female breasts is presented. As always, Outlander has a good deal to say about the topic!
FIRST the STATS: Well, there are lots of statistics and none are encouraging: breast cancer is the most common cancer of women both in developed and less developed countries – surprisingly, almost 50% of worldwide breast cancer cases occur in underdeveloped nations. An estimated 12.4% of US and 12.5% of UK women will be diagnosed with breast cancer at some point during their lifetimes. As for the guys: expectations are that one in 1,000 US and one in 870 UK men will be diagnosed with breast cancer during their lives.
Bottom Line: So, why an anatomy lesson on the breast? Understanding breast anatomy can help parents appreciate challenges and rewards of breast feeding and to help male and female patients discuss signs and symptoms of breast diseases as well as treatment options more fluently with health care providers. Useful? I certainly hope so!
Purpose: Based on western culture, one might rightly assume the breast was created to sell merchandise, garner attention, promote discrimination, induce titillation (no pun intended), or sexual arousal. From a biological viewpoint, the purpose of the female breast is for milk production, a process known as lactation… Sometimes a cigar is just a cigar! ?
Outlander Abundance: Our fav book and TV series often pay homage to both male and female breasts…. equal opportunity entertainers! A quick survey reveals breasts in most Outlander episodes:
- Jamie: ep 102, 104, 105, 106, 107, 109, 110, 112, 116, 201, 202, 204, 206, 208, 211
- Claire: ep 101, 102, 107, 108, 109, 110, 204, 206
- Jenny: ep 102, 114
- Frank: ep 101, 106
- Geillis: ep 110, 111
- Angus: ep 108, 209
- Rupert: ep 209, 210
- BJR: ep 116
- Louise de la Tour: ep 202
- Dougal: ep 209 (we waited a long time for this one!)
- King’s mistress: ep 202
- Suzette: ep 203
- painted woman at Madam Elise’s brothel: ep 203
Not that I am keeping track <g> but no male or female breasts were shown in episodes 103, 113, 115, 205, 207, 212, 213 (Did I miss any?)!
Diana liberally honors breasts and nipples throughout her works. There are so many examples in the Outlander book series, not enough room to list in this lesson. If I recall correctly, even her spouse once commented something like, “nipples again?” But, I am not complaining! So, let’s go!

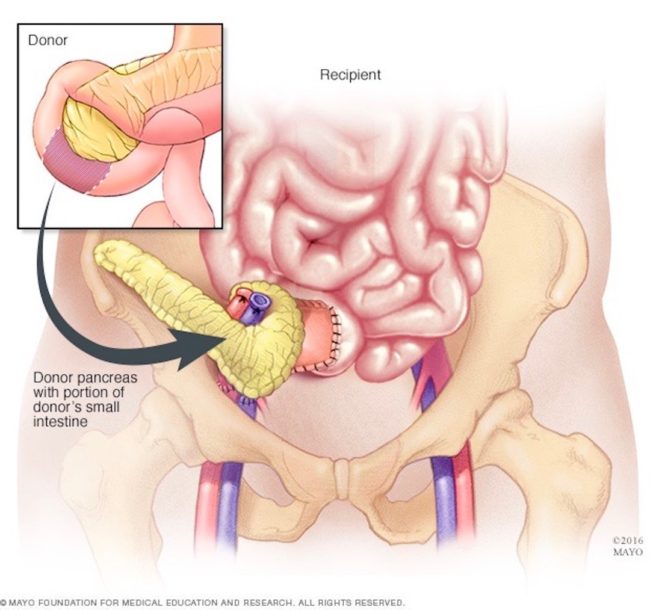
Anatomy of the Male Breast: First the guys!
What better model of the male breast than Jamie? A moment of silence for this fab lad in appreciation for the hard-earned state of his body. With very little body fat, breast contour can be rightly attributed to thorough development of chest muscles (ep 106, The Garrison Commander).

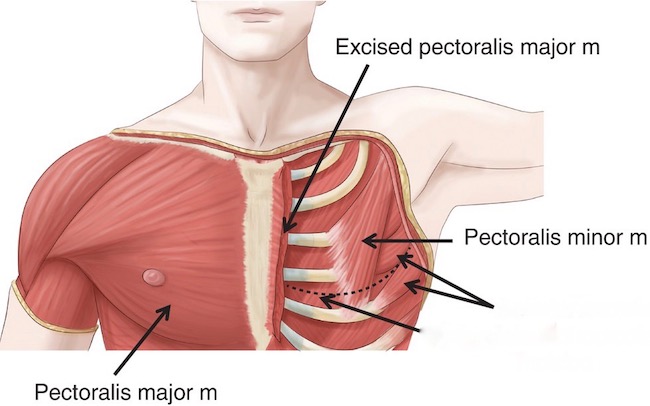
Position: Male breasts sit atop the chest wall (Image A), a sturdy musculoskeletal base including ribs and intercostal muscles (Anatomy Lesson #15, Crouching Grants – Hidden Dagger), pectoralis major and pectoralis minor muscles (Anatomy Lesson #4: Jamie’s Chest – 8th Wonder of the World!). These are layered as follows: pectoralis major is most superficial; pectoralis minor lies deep to pec major; and, ribs and intercostal muscles (Image A -single arrow) are deep to pec minor.
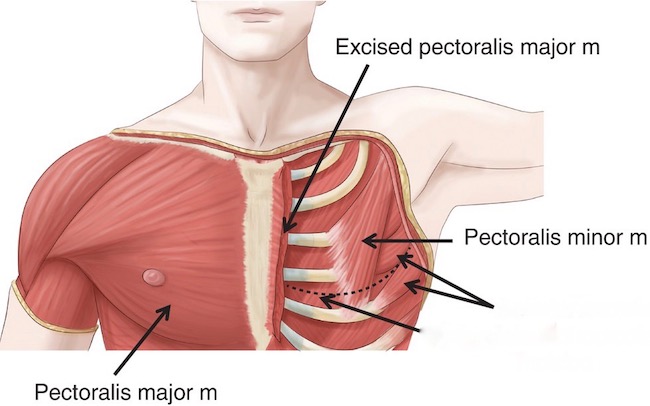
Image A
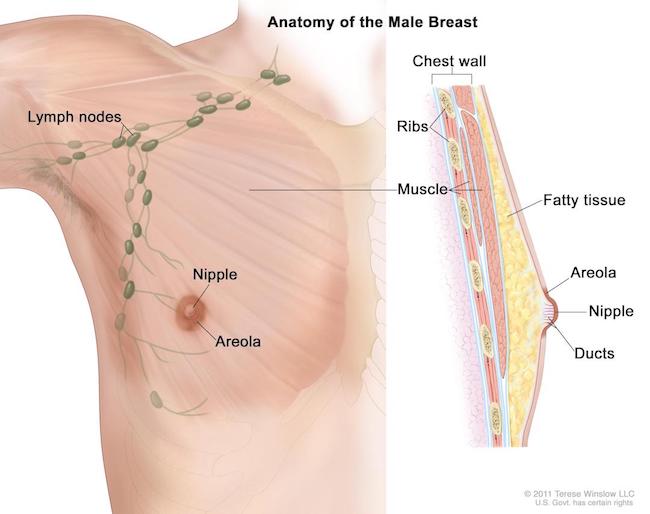
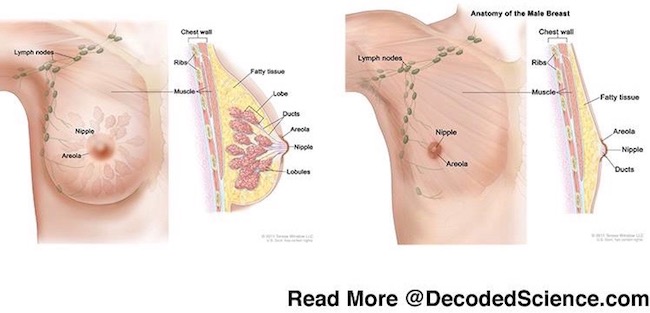
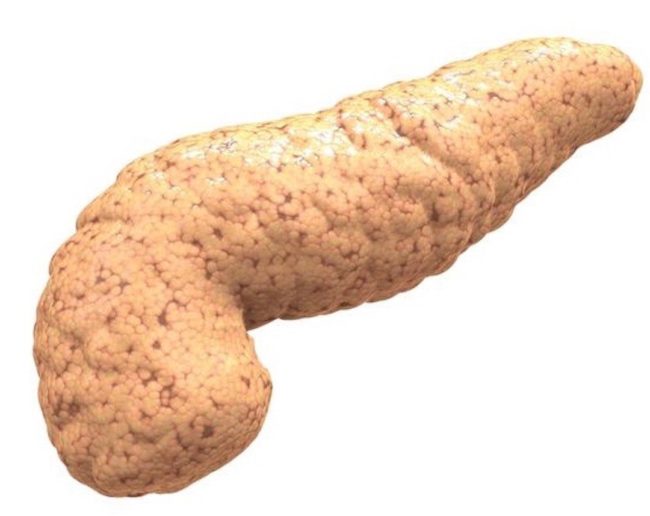
Breast Parts: The male breast includes the following parts (Image B):
- nipple (pigmented elevation)
- areola (pigmented ring around nipple)
- ducts (leading nowhere)
- fat (variable)
Nipple and Areola: Both highly pigmented structures, the areola surrounds the nipple. BTW, areola is pronounced əˈrēələ, not ar-e-o’-la.
Ducts: Ducts (yes, men have them) underlie the nipple and areola but are typically rudimentary and nonfunctional (Image B – right view).
Fat: The amount of fat in the male breast usually reflects over body fat deposition. Generally, more breast fat accompanies a higher BMI (body mass index).
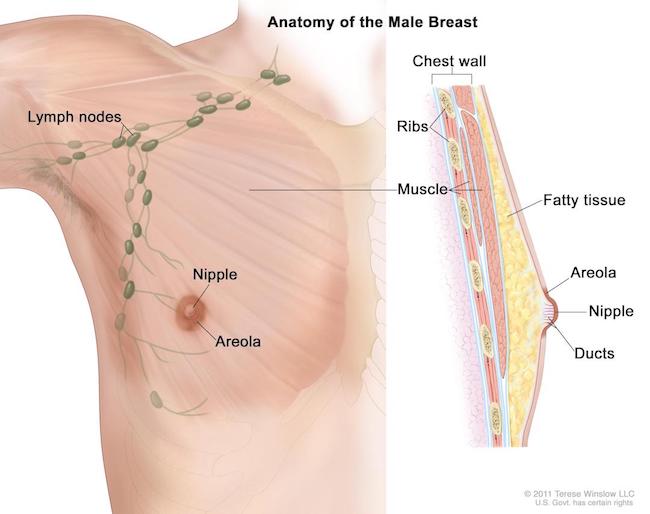
Image B
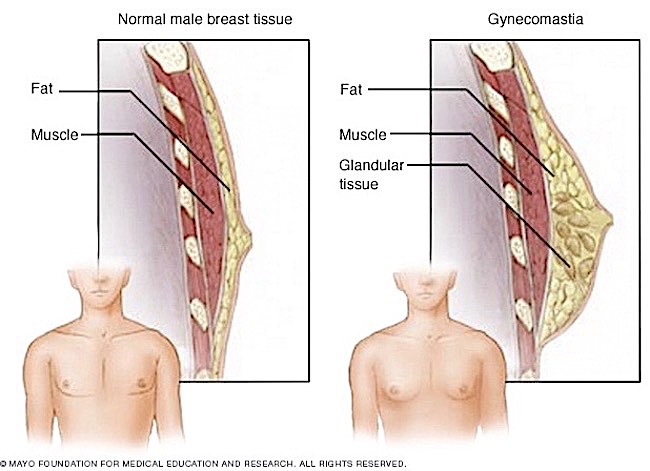
Gynecomastia: Of current concern is male gynecomastia, defined as an increase in the size of male breast tissue (Image C). Gynecomastia is triggered by a relative decrease in the amount of testosterone compared with estrogen levels. Although estrogen is considered the female hormone, men normally produce it in small quantities. However, if male estrogens are too high or out of balance with testosterone levels, then gynecomastia may occur.
Infants: More than half of male infants are born with enlarged breasts due to exposure to their mom’s estrogen. This usually resolves within 2-3 weeks after birth.
Puberty: Hormone changes during puberty not uncommonly causes gynecomastia. Again, this usually resolves within 6 months to 2 years.
Men: Prevalence of gynecomastia peaks between 50 and 69 yrs. and may be influenced by many agents which cause glandular tissue to develop from the rudimentary ducts (Image C – right side):
- various anti-androgen compounds used for cancer treatment
- some medications for AIDS, heart, gastric motility, and ulcers
- some anti-anxiety and antidepressant meds
- some street drugs, alcohol
- some herbal products
- aging
- liver failure
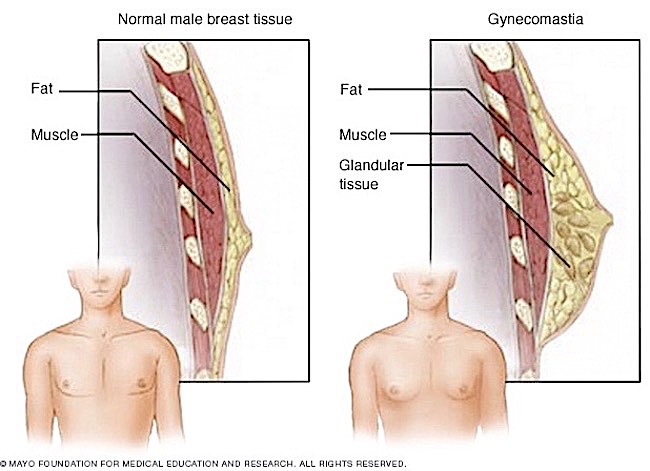
Image C
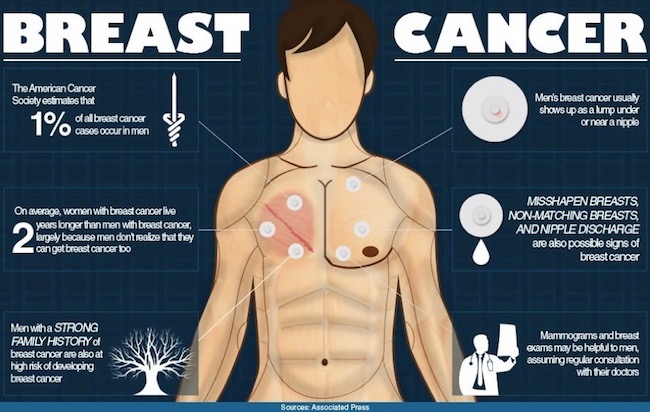
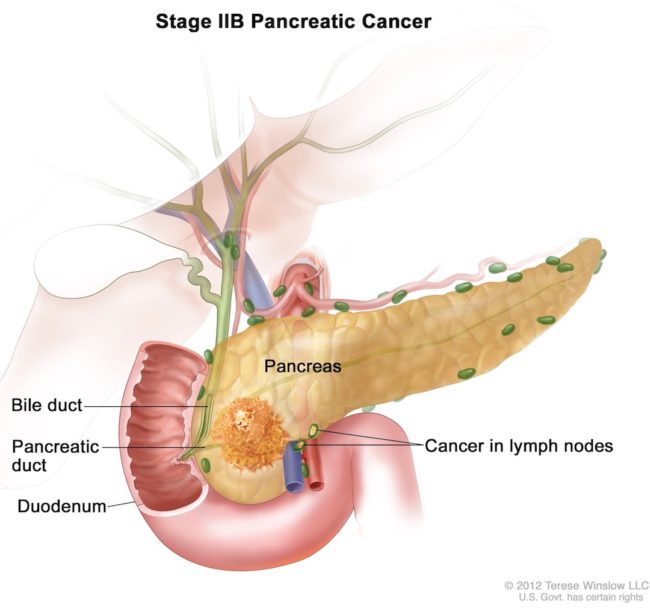
Male Breast Cancer: Now for a crucial topic no one likes to consider. Many people do not realize men have breast tissue and can develop breast cancer! Breast cancer is a malignant tumor that starts from cells of the breast. Breast cancer cells may grow into (invade) surrounding tissues or spread (metastasize) to distant areas of the body. The following image is a great summary of risks and signs of male breast cancer (Image D)! Please check these out. Many do not realize that like women, men may have a familial disposition to breast cancer. Truth!
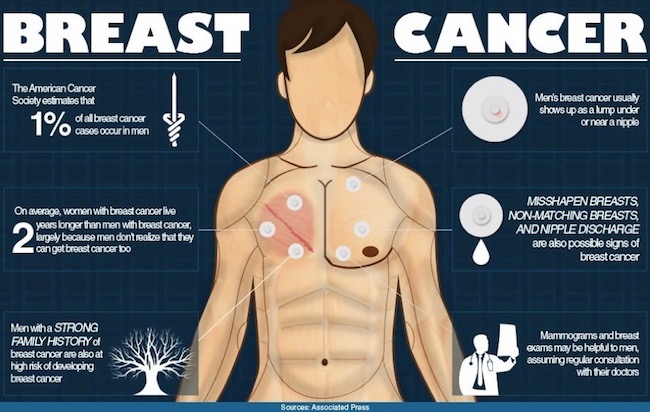
Image D
True Story #1: Why do males have breasts? As an anatomy professor, I always champion the position that the body doesn’t have useless structures. Once, a particularly astute student asked in class: “then, why do men have nipples?” Hum….well, I must confess, this kind of stumped me! I pondered the issue and have conclude that men have nipples/breasts for developmental protection. This is my thinking: it is much easier for genetic machinery to produce one sex with fully developed breasts and one sex with underdeveloped breasts than it is to produce one sex with fully functional breasts and the other sex with zip on the chest wall! The latter would add layers of genetic complexity, openly inviting more developmental challenges than our current states of being. Thus, I still hold to my original position! Please feel free to challenge me on this. Je suis prest!
Anatomy of the Female Breast: Now, for the gals!
You might think it only fair that as Jamie is used as the model for the male breast, I will use Claire for the female counterpart. But, I am not going to be fair. Just too intrusive. Sorry to disappoint, but the episodes are listed above for you to view and review! <G>
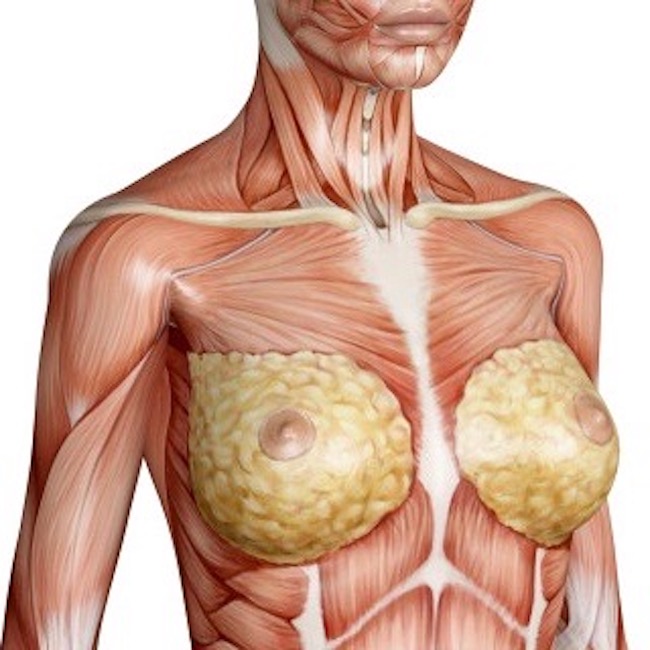
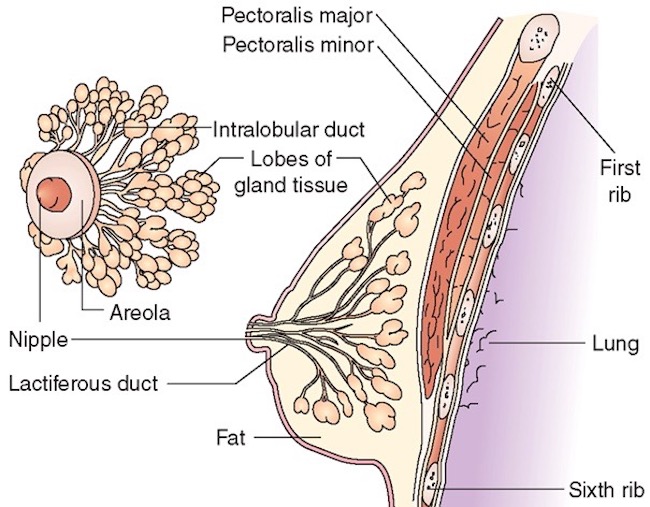
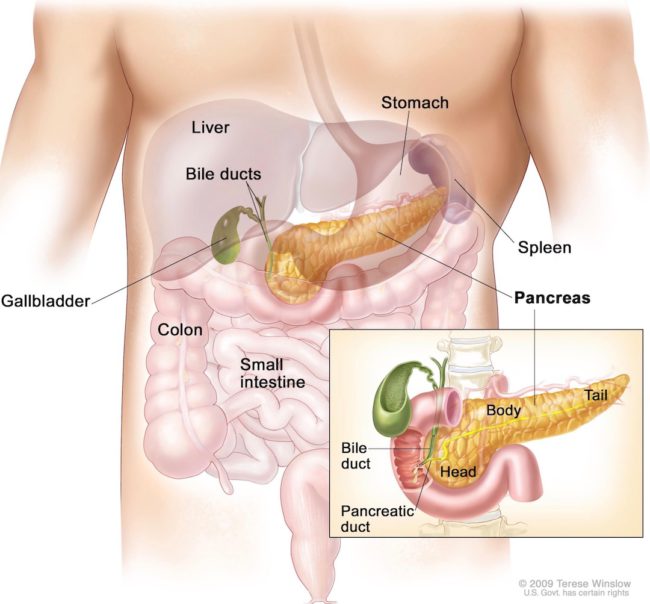
Location: This goes without saying (but, I will anyway), female breasts are typically more developed than male breasts. But, the relationship to chest wall remains the same: female breasts are superficial to pectoralis major muscles (Image E) and are separated from the muscles by a tough connective tissue layer called fascia.
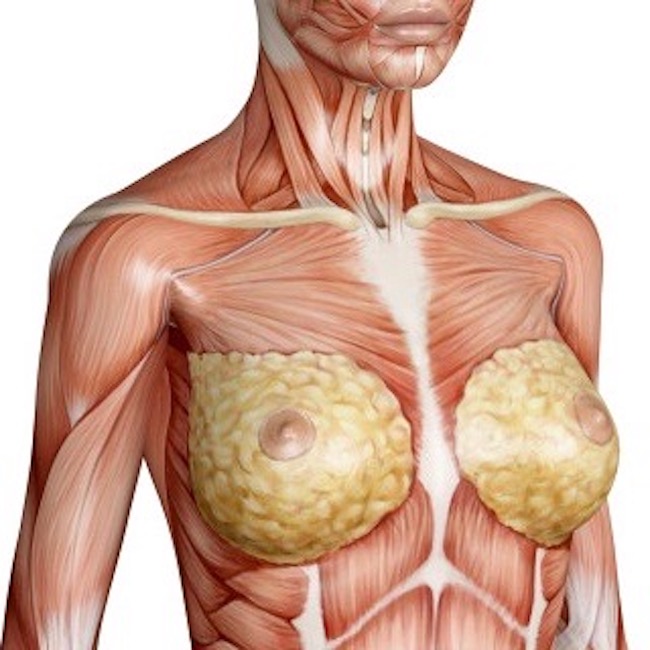
Image E
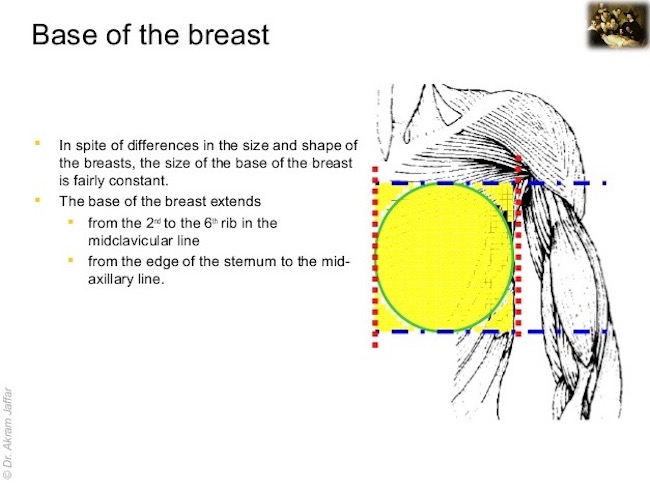
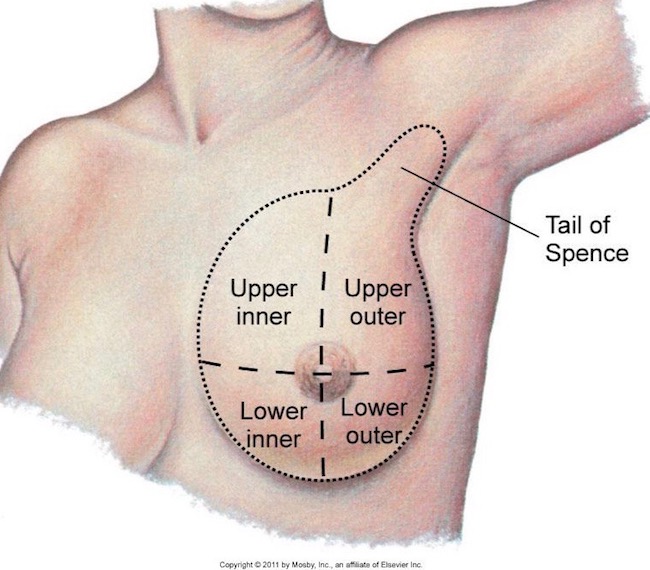
Base of Breast: Variations in size, shape, and symmetry of female breasts are the rule, not the exception – even between the breasts of the same person. But, the base of breast, the site where it attaches to the chest wall, is amazingly consistent among women (Image F). The base is located:
- vertically, 2nd to 6th rib (Image F, between blue dot/dash lines)
- horizontally, edge of sternum to side of torso (Image F, between red dotted lines)
Try This: Wonder where the 2nd rib is? Place a finger in the suprasternal notch, the divot at the top of your breast bone (Anatomy Lesson #13, Crouching Grants – Hidden Dagger). Move finger downward about 2” (5 cm) until you encounter a prominent bump on the sternum; this is the sternal angle of Louis – and the same level as your 2nd rib. Now, run finger down to tip of the sternum; the 6th rib lies about 1” (2.5 cm) above the tip.
Next, run finger from edge of sternum to midway on your side; this is the horizontal extent of the base of breast. Now, you have a good estimate of the base of breast no matter how large or small the cup size!
Breast Exam: Most women and some practitioners might not know the full extent of breast tissue. A thorough breast exam should explore the full base of breast as well as all remaining breast tissue!
True Story #2: A dear friend found a lump high up by her second rib. A high-grade breast cancer, she is now six years out and doing well as it was caught early and treated aggressively. She now rows in dragon boat races around the world. Moral: check the breast base!
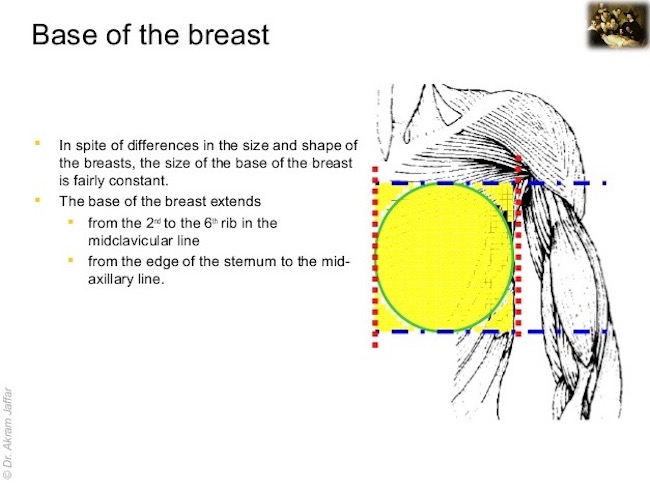
Image F
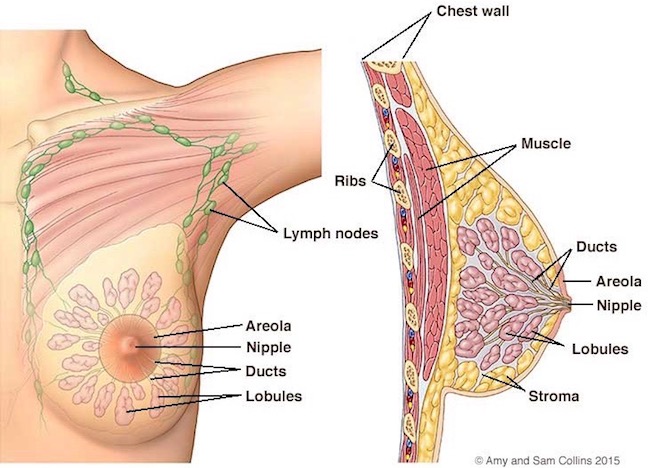
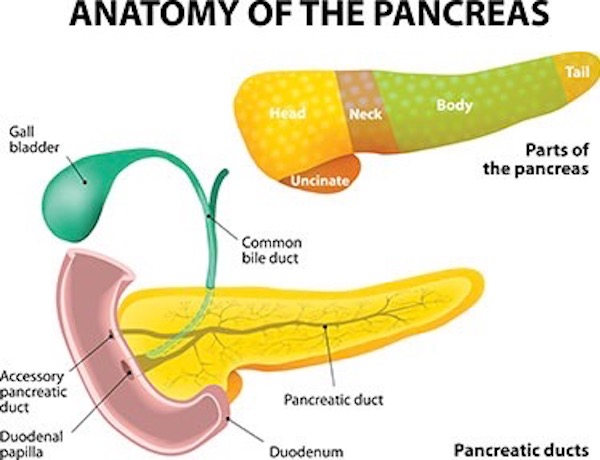
Parts: Female breasts have the same parts as males with the addition of well-developed glands, ducts and fatty tissues (Image G).
- nipple
- areola (pigmented ring around nipple)
- smooth muscle
- lactiferous ducts (lead from glands to nipple)
- mammary glands (drain into ducts during lactation)
- fat (variable amounts)
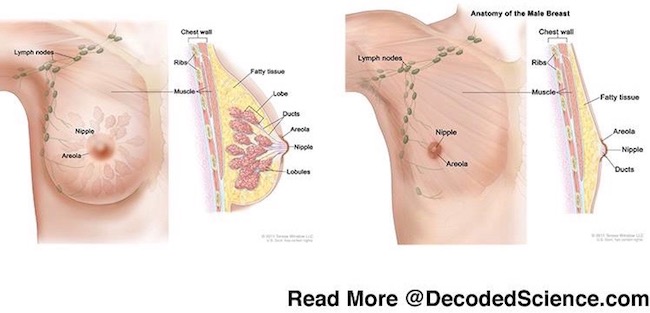
Image G
Nipple-Areolar Complex (NAC): NAC is an anatomical acronym for nipple and areola; both are generally well-developed in females.
The nipple is large, (usually) elevated, hairless, and heavily pigmented with melanin (Anatomy Lesson #5, Claire’s Skin – Opals, Ivory, and White Velvet). Nipple skin is thicker than most other skin, designed to resist wear and tear during nursing (Image H). In males and lean or nulliparous (no birth) females, the nipple typically overlies the 4th intercostal space (between ribs 4 and 5) but this is unreliable in women who have given birth at least twice or who have heavy breasts.
The areola (from Latin area meaning “small, open space”) is the region encircling the nipple; it is essentially hairless, slightly raised, thick skinned, and more heavily pigmented than surrounding skin (Image H). The areola usually darkens during pregnancy, retaining the increased pigmentation thereafter. Scattered surface bumps are glands of Montgomery, specialized sebaceous glands (Anatomy Lesson #5, Claire’s Skin – Opals, Ivory, and White Velvet) which release oily substances to water-proof nipple and areola and keep them pliable. Some anatomists posit that the pigmented areola and nipple give the nursing child a target to aim at! Hah!
Jamie is verra knowing about the areolae (pl.). Here from Outlander book:
“That,” I said primly, “is an areola, and you know it, because I told you last week.” “So ye did,” he murmured. “And there’s another one, fancy that.” The bright head dipped to let his tongue replace the finger, then traveled lower.
Thud!

Image H
Smooth Muscle: Finally, the dermis deep to NAC contains specialized bundles of smooth muscle cells (visible by microscopy) – a type of involuntary muscle we studied in Anatomy Lesson #45: Tremendous Tube – GI System, Part 2. Contraction of smooth muscle bundles erects the nipple and tightens the areola. Biologically speaking, this response gives a more substantive bud for an infant to suckle. Nipple erection is managed by the autonomic nervous system, an involuntary response over which even actors have no voluntary control (Starz episode 107, The Wedding)! <GGG>

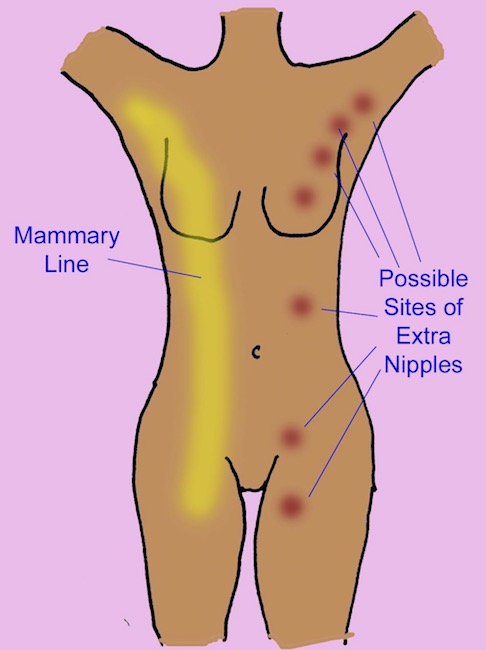
Supernumerary NAC: This is for fun: humans may exhibit supernumerary NAC. These are typically located somewhere along the milk lines, a pair of lines extending from armpits through breasts, down the abdomen, and ending near the anus (Image I). Animals, such as cats and dogs, have multiple nipples along the milk lines. However, supernumerary NAC in humans can be found pretty much anywhere!
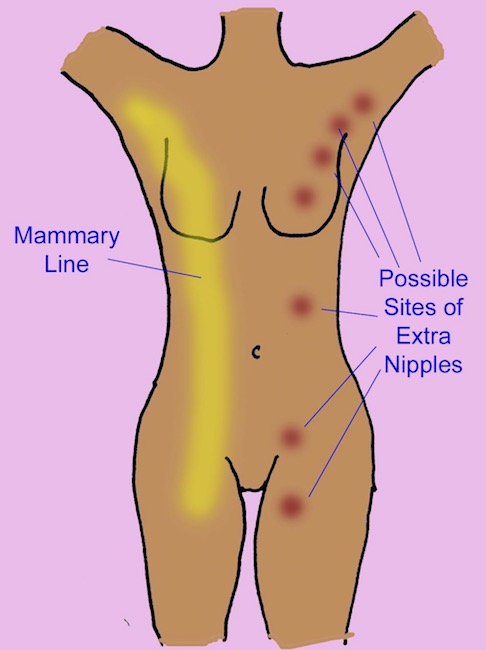
Image I
Apparently, seven celebrities claim to have supernumerary nipples, and purportedly belong to the so-called Triple-Nipple-Club! Snort! Image J, however, is a highly unusual site for a supernumerary NAC (owner unknown). I cannot image that this location would, in any way, prove comfortable or useful other than an entertaining ice breaker at a cocktail party!

Image J
Back to the dissection table!
Lactiferous Ducts: Mammary glands are arranged into 10-20 lobules (small lobes) arranged around the NAC. Each lobule is drained by its own lactiferous duct. All ducts converge near the nipple. Here, each duct expands into a tiny reservoir, a small holding tank for milk to accumulate between swallows by a nursing infant. Again, each duct extends from its lobule to the nipple, resembling the spokes of a wheel (Image K).
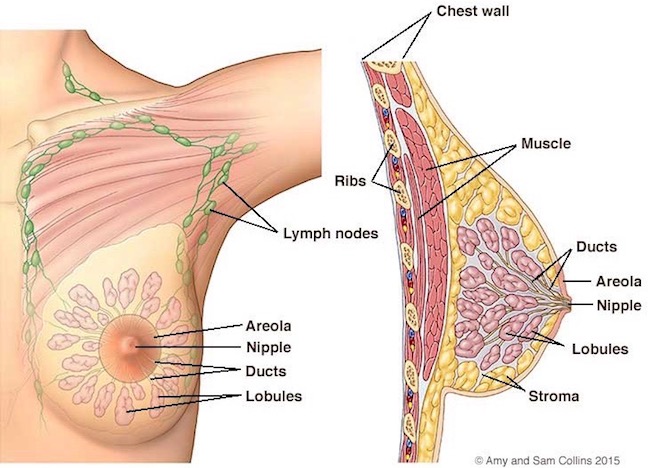
Image K
Nipple Openings: Some folks don’t realize that 10-20 ducts open onto the surface of the nipple – each lactiferous duct has its own opening. Years ago when breast feeding was out of vogue (?), old style bottle nipples bore a single opening and peeps who weren’t exposed to breast feeding had no clue that this in no way mimicked the human breast.!
Probably most fans are aware that Jenny was wearing a very convincing prosthesis and pump in Starz episode 114, The Search. This prosthesis illustrates the assumption that a single duct opens onto the nipple, but this is not so.
True story #3: After episode 114 aired, a fan messaged me stating that his wife was breast feeding and human milk doesn’t eject from the breast as it did with Jenny. Actually, it can and does. Breast milk may ooze, drip, or even spurt like a fountain. Truly amazing!
If this info surprises you, dinna fash! Even Nurse Claire didn’t know the female breast can performs such wonders (Outlander book). Diana kens!
“I canna leave the babe for long,” she said in answer to my thoughts, grimacing as she cupped one breast from beneath. “I’ll burst.” In response to the touch, milk had begun to drip from the engorged nipple, thin and bluish. Pulling a large kerchief from her pocket, Jenny tucked it beneath her breast. There was a small pewter cup on the ground beside her, one she had taken from the saddlebag. Pressing the lip of the cup just below the nipple, she gently stroked the breast between two fingers, squeezing gently toward the nipple. The milk dripped faster in response, then suddenly the areole around the nipple contracted and the milk spurted out in a tiny jet of surprising force.
“I didn’t know it did that!” I blurted, staring in fascination.
Forgive Claire, she is a combat nurse and breast feeding is an likely maneuver on a battlefield. I love that Diana doesn’t shy away from the human body with its array of marvelously, messy functions – a courageous example to all. And, ditto to our Jenny actress – remember, no names!

Nipple Piercing: Hum…. I am not a huge fan of nipple piercing, despite its popularity, as the large bore needle used for piercing and hefty nipple rings may cause a strammash with anatomy of the lactiferous ducts (Image L). ‘Nuf said!

Image L
Murtagh, on the other hand, was perfectly fine with Piercing Practices – one of the few times we see Godfather crack a smile (Starz episode 202, Not in Scotland Anymore). Hurry, Murtagh. Back to the Paris apartment and Suzette!!!
Of course, Dragonfly in Amber book says Jamie’s (not Murtagh’s) eyes were watching the swinging swans!
She was, in current vogue, wearing a gown cut below both breasts… The breasts of “Nesle,” while reasonably adequate in size, pleasant in proportion, and tipped with large brownish areolae, were further adorned with a pair of nipple jewels that caused their settings to recede into insignificance. A pair of diamond-encrusted swans with ruby eyes stretched their necks toward each other, swinging precariously in their gold-hooped perches. The workmanship was superb and the materials stunning, but it was the fact that each gold hoop passed through her nipple that made me feel rather faint. …I felt a presence in my rear and stopped just in time to avoid backing into Jamie, who was watching the King’s mistress with no pretense whatever of tactful obliviousness. “She told Marie d’Arbanville that Master Raymond did the piercing for her,” I remarked under my breath. His fascinated gaze didn’t waver.
Hah! I just bet those bonny blue orbs stayed focused!

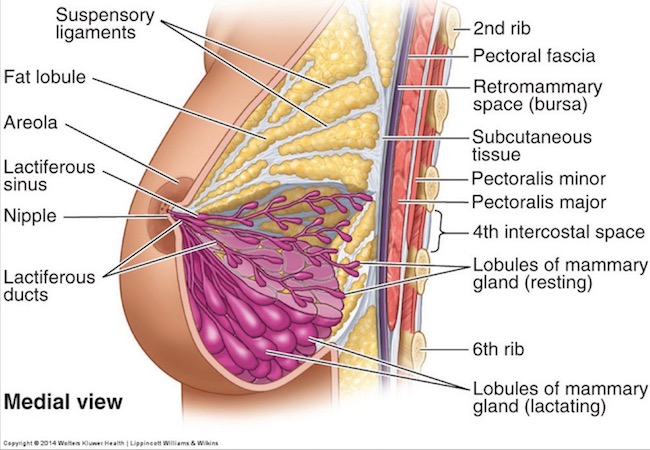
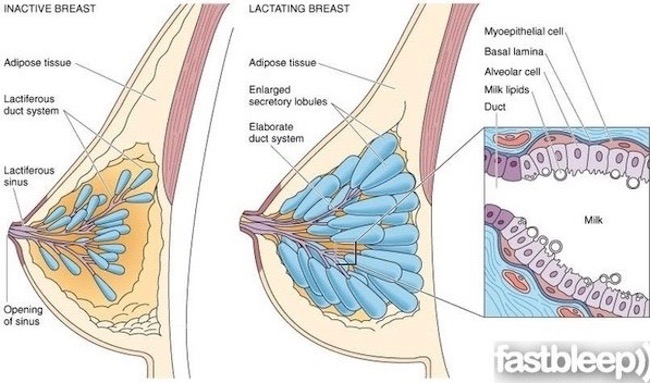
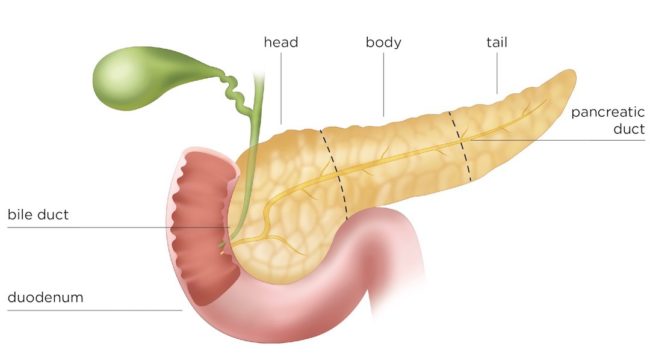
Resting Breast: Now, to the nitty-gritty: mammary glands are a specialized type of sweat gland. Yep, ’tis true! A quiescent (non-lactating) breast typically doesn’t have much glandular tissue but that present is organized into 10-20 lobules, each drained by its own lactiferous duct, as described above. Most bulk of a non-lactating breast is adipose tissue (fat, but adipose sounds soooo much bettah!).
Here’s something really important! Most breast illustrations inaccurately show glandular tissue evenly distributed around the NAC (Image M). And, old-style breast implants look like half a baseball pushed under the skin, which is also incorrect! These appear odd to the eye because the natural breast is tear-drop shaped: outer and bottom breast borders are well-defined, but inside and top borders slope from chest wall toward the NAC, producing to the tear-drop shape. More importantly, breast glands are also distributed in a tear-drop configuration!
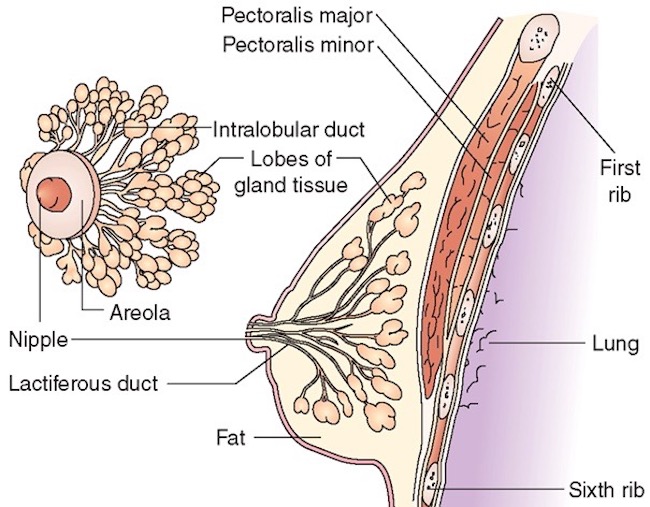
Image M
Axillary Tail: Breast glands do surround the NAC, but a tail of glandular tissue extends up towards the axilla (armpit), the so-called axillary tail of Spence (Image N). Divide the breast into four quadrants and see the glandular tail extends from the upper outer quadrant toward the axilla. Ergo, like the base of breast, this area must be included in a thorough breast exam! This is why mammography technicians work very hard to mash and smash the entire breast between those plates!
Try this: On yourself or a willing (very important!) female partner, grasp the anterior axillary fold (Anatomy Lesson #4, Jamie’s Chest – 8th Wonder of the World), this fold of pectoralis major muscle lies just in front of the armpit. Feel the flesh overlying this fold – the axillary tail is in the overlying flesh. Breast tissue feels slightly bumpy-lumpy under the fingertips. Confirm its continuity with the rest of the breast tissue. This is the axillary tail. Good job!
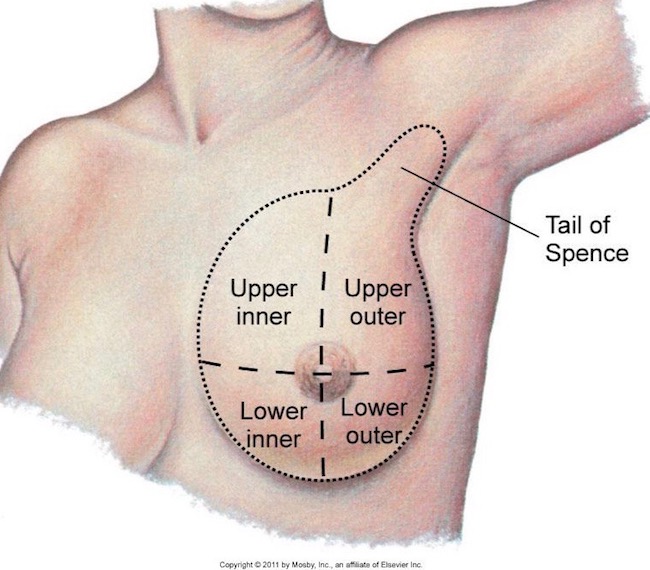
Image N
Fat and Connective Tissue: The female breast typically contains fat insinuated between gland lobules and ducts (Image O) – the amount is highly variable. In a quiescent breast, most of its size is dictated by fat deposits and these are regulated by hormones because fat is required to convert precursor molecules into estrogens.
Fat, ducts, and glands are supported by the suspensory ligaments of Cooper. Suspensory, my sporrin! These dinky strands of collagen should never share the same name with those splendid, stout bands of collagen lending integrity to most of our joints! Typically, the suspensory ligaments are so wee and weak, they can barely be found during dissection! Believe me, they are much thinner than Image O suggests. And, they offer basically zip support for larger breasts!
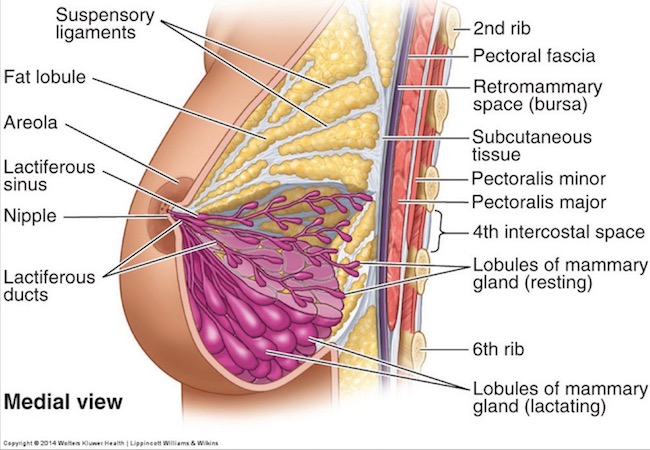
Image O
Active Mammary Glands: During pregnancy, three hormones (estrogen, progesterone, human placental lactogen) stimulate breast gland growth. Rapid gland grown arising from the lactiferous ducts and enhanced fat deposition account for a dramatic increase in breast size (Image P) when a little one is in the oven. Imagine the budding of blossoms from a tree branch as a splendid analogy to gland development of the breast!
After birth, progesterone and estrogen levels fall and the anterior pituitary gland releases the hormone, prolactin, stimulating the breast to produce milk.
Lactating mothers often experience the “let down” reflex, a tingling, tightening, or warm feeling in the breasts after an infant begins to suckle. Once conditioning sets in, some moms just think about nursing her child, and down the milk comes! This response occurs because another hormone, oxytocin, released from the posterior pituitary gland, targets specialized cells around lactiferous glands and ducts. Oxytocin causes these specialized (myoepithelial) cells to contract which moves the milk along the duct system towards the NAC (Image N – right panel). This amazing process is clearly designed to ensure our young are effectively nurtured.
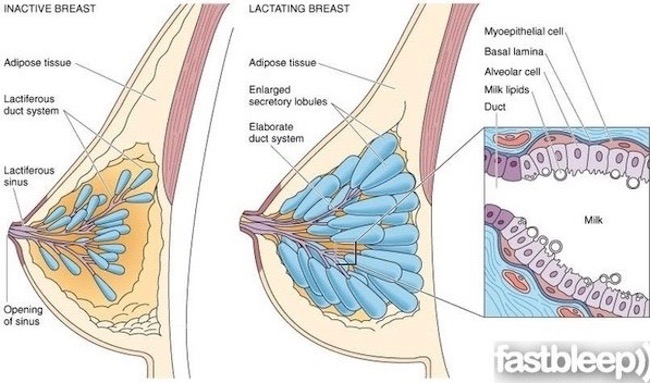
Image P
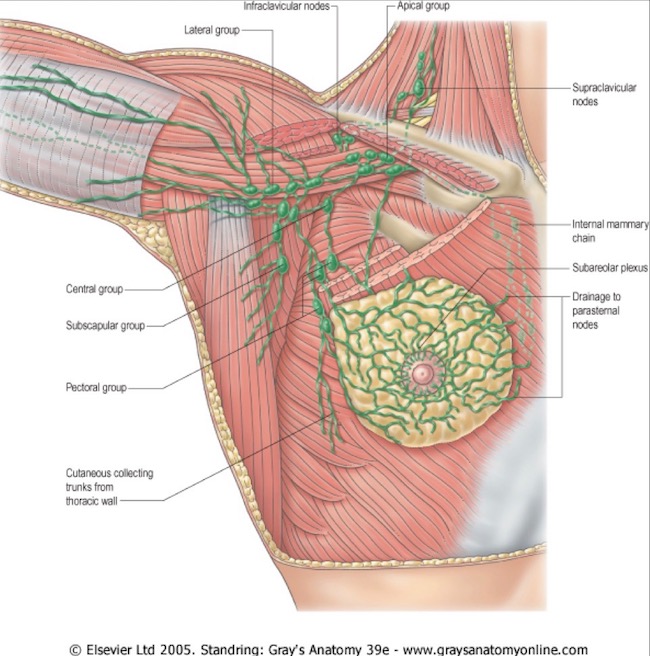
Breast Lymphatics: I have yet to write a lesson about the amazing lymphatic system. So, in a nut shell, almost all body tissues (a few exceptions) are riddled with lymphatic vessels which collect fluid escaping from small blood vessels. Next, the fluid enters lymphatic vessels as lymph and is subsequently returned to the blood vascular system. This cooperation between two circulatory systems prevents our tissues from swelling with too much accumulated fluid.
Male and female breasts are riddled with lymphatic vessels (Image Q; male shown in Image B ), draining lymph towards arm pit or top of chest or crossing to the midline. Along the way, lymph percolates through several groups of lymph nodes. These tiny organs contain protective cells which surveil the fluid, removing undesirables (cancer cells, pathogens, foreign matter, etc.) from the lymph. They also help mount immune responses to destroy unwanted antigens in the lymph.
Although this design ensures that excess fluid is removed quickly and efficiently, especially during lactation, it also allows for metastases of breast cancer. Cancer cells love to jump ship and enter the lymphatics. If they escape surveillance by protective cells of lymph nodes, they continue to hitch a free ride spreading to other body sites.
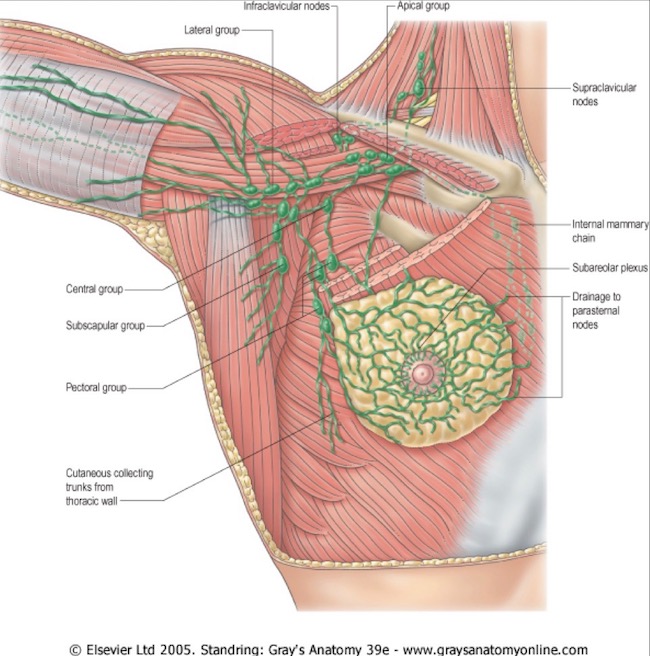
Image Q
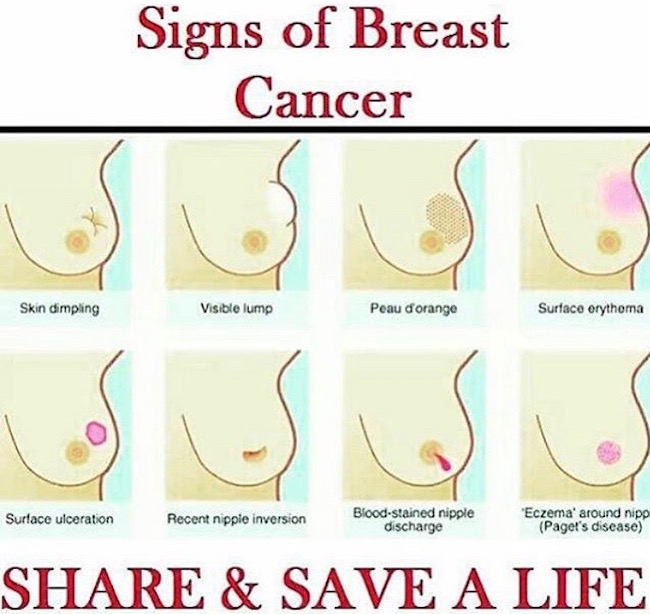
Female Breast Cancer: Returning to this unhappy but crucial topic, the female breast exhibits more signs and symptoms of this dreadful disease because it is more developed (Image R)! Unfortunately, the eight signs shown in Image R tend to appear rather late in the course of a cancer. You should also know that breast cancer isn’t one disease; there are at least five main types with several grades among the types. Thus, it is crucial that women perform self-exams and get breast checks on a regular basis. Please be aware of these signs, be vigilant, and follow your health care professional’s guidelines! (BTW, peau d’ orange means “orange peel skin”)
True Story #4: Many men and women who experience open breast biopsies may wait many days for a path report and diagnosis. I worked with a pathologist, board certified in FNA (fine needle aspiration), who specialized in diagnosing breast disease. He pushed a cart loaded with stains, microscope, etc., into the room of his patient; aspirated the lump with a needle, prepared the specimen, viewed it under the microscope, and gave the patient a diagnosis on the spot. No agonizing waiting. No scar. If you are told you need a biopsy, think about requesting a FNA.
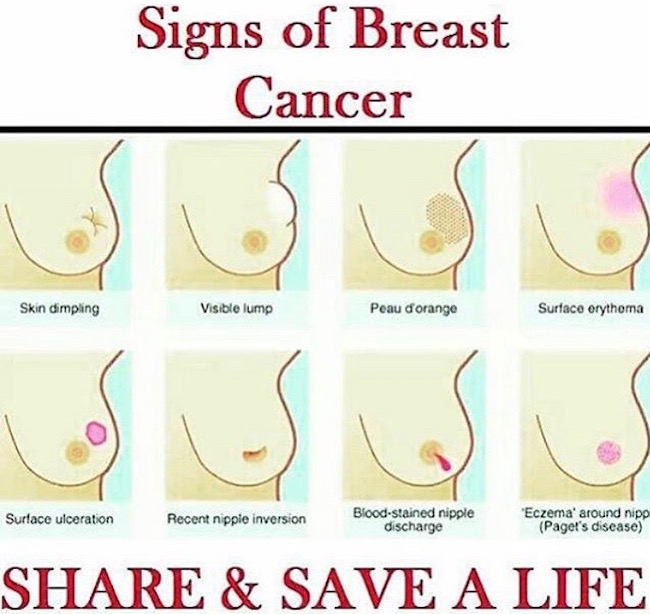
Image R
OK, anatomy of male and female breasts is done. Time for a wee bit more fun!
True Story #5: Recently, a reader asked me why breasts appeared so high and rounded as seen with many Outlander costumes. I think she intends something like Claire’s glorious wedding dress (Starz episode 107, The Wedding) – the one for her marriage to Jamie, not the 40’s suit she wore to marry Frank! This appearance doesn’t occur because breast anatomy somehow morphed over 200-300 years; breasts assume this shape because of the corset!

Recall this scene (Starz episode 102, Castle Leoch)? After much grunting, huffing, and puffing, Mrs. Fitz trusses Claire up like a Christmas goose! Comfortable, Sassenach lass? I shouldna think so!

Diana explains in Outlander book:
Brooking no protests, the dame bustled me out of my inadequate garments and oversaw my dressing from the skin out. She stood back, surveying her handiwork with satisfaction.
In the episode, Claire modestly removes her “French brassiere” and panties under the disapproving eyes of Mrs. F! They were replaced with bum roll, shift, and corset, which flattens the breasts, because it has no cups.

Even Laoghaire gets into (erm, almost out of) the act… (Starz episode 109, The Reckoning) – her goose flesh literally honks! And, I want to know how those laces made their way to the front of her corset? And where did she find it? Bet granny Fitz didna ken Laoghaire was into Castle Leoch’s fab closet! Grrrrr! (Love the actress, though!).

I am not a costumer and I may hear back from those who are. But, I believe 18th century corsets usually covered the breasts (or barely did, as with the teen trollop), or ended under the breasts, or had primitive, sewn-in cups. A corset like Claire’s was typically laced as tightly as possible, flattening breasts against chest wall. Where does a healthy breast go? Well, having little choice, it pops up over the corset top, hence the robust (Get it? – robust?) effect of Claire’s gorgeous wedding gown!
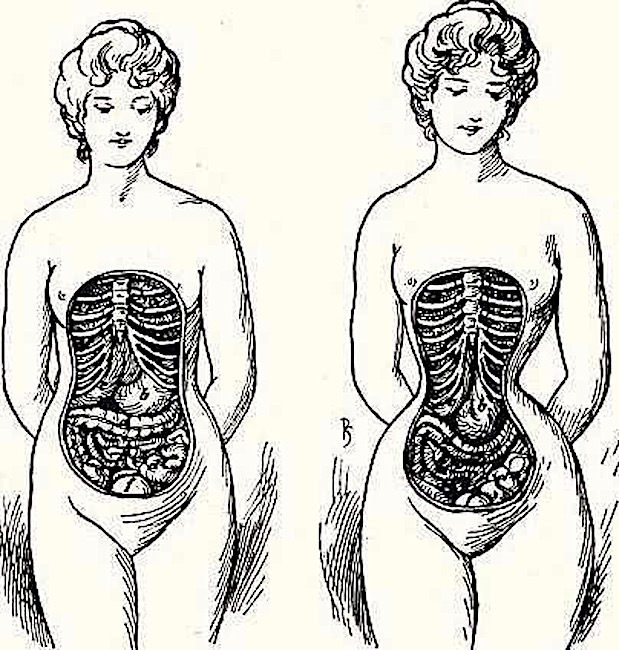
If the waist was laced tightly, an hour-glass figure emerged, highly desirable, especially in the 1800s (Image S)! But, that squeeze was pretty rough on rib cage and internal organs….which brings me to the next story!
True Story #6: When I was in graduate school, my anatomy professors claimed that 18th and 19th corsets compressed internal organs so much that, upon autopsy, the livers of some women were permanently grooved by compression against the ribs. You get the idea in Image S. A good story, but one I have not been able to confirm as true or false.
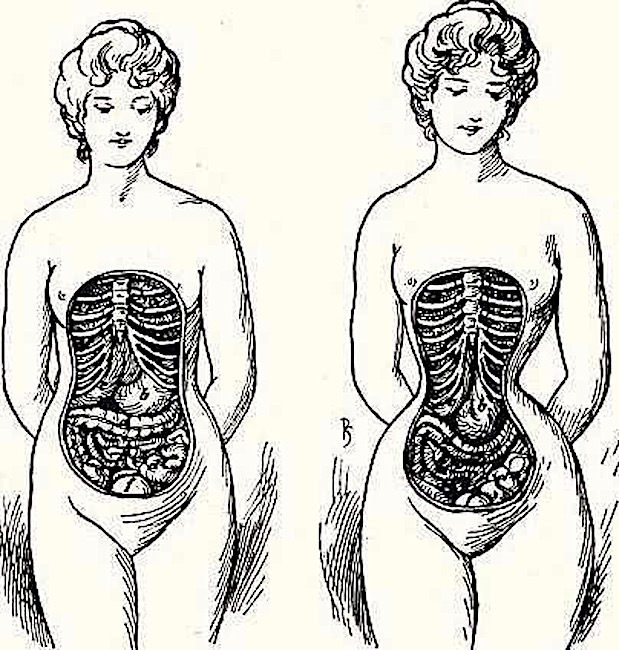
Image S
Thus ends the fascinating saga of human breast anatomy. Darn! Wasn’t it interesting? Do we now understand the basic anatomy of male and female breasts? Hopefully, yes, but this is unlikely to alter their rather universal appeal!
Let’s close with an evocative, contemporary ode to her breasts. Written in June of 2015, apparently, it is based on a true story!
Her Breasts (Mammary Memory)
by Joe Cottonwood
The white-haired doddering gentle old man
in the crushing silence of the public library
blinking through spectacles
writes with shaking hands
in a pocket notebook
unaware that he is muttering to himself:
Her breasts… her breasts…
Eyes peer over books. Pencils pause,
except the old man’s. Fingers
mark pages. We await,
expectant, puzzled. He has pulled a dusty volume
from the shelf of his memory
and still writing, whispers, hissing:
Her breasts…
I want to know: was it in moonlight?
Hurried? Forbidden?
Dear woman, take joy that after half a century
not only your lover but a whole reading room
of men and women are sharing — are in awe of —
your stunning warmth:
Her breasts! Her breasts!
A deeply grateful,
Outlander Anatomist
Photo Creds: Starz, Gray’s Anatomy for Students, Drake, Vogl and Mitchell, Elsevier, 2005 (Image H), www.bolatitoblog.com (Image R), www.cambridge.org (Image A), www.cancer.gov (Image B), www.cancerworld.info (Image D), www.causticsodapodcast.com (Image J), www.diariosanacronicos.com (Image S), www.healthtype.com (Image E), www.komennyc.org (Image K), www.decodedscience.org (Image G), www.mayoclinic.com (Image C), www.quora.com (Image P), www.reddit.com (Image I), www.slideshare.net (Image F), www.studyblue.com (Image N; Image O; Image Q), www.theronion.com (Image L), www.what-when-why-how.com (Image M)