
We miss ye already yoo ever lovin’ goof! Join Anatomy Lesson #41 tomorrow, as we bid Angus adieu.
A deeply grateful,
Outlander Anatomist

Human Anatomy taught through the lens of the Outlander books by Diana Gabaldon and the Starz television series

We miss ye already yoo ever lovin’ goof! Join Anatomy Lesson #41 tomorrow, as we bid Angus adieu.
A deeply grateful,
Outlander Anatomist
Welcome Outlander Anatomy readers! Our last lesson covered the human skeleton (Anatomy Lesson #39 “Dem Bones – The Human Skeleton”). Today’s Anatomy Lesson #40, “Snap, Crackle, Pop! or How Bones Heal” expands on bone anatomy but also addresses bone fractures and how they mend. As always, Starz Outlander images and quotes from Diana Gabaldon’s marvelous books are generously sprinkled throughout the lesson.
Last lesson began with spectacular images from Master Raymond’s hidden ossuary. This lesson, we start with images of a world famous ossuary located in Kutná Hora, Czech Republic. Known world-wide as the Bone Church, it is an ossuary (‘Kostnice’ in Czech) that houses the bones of an estimated 40,000 – 70,000 people (Image A).
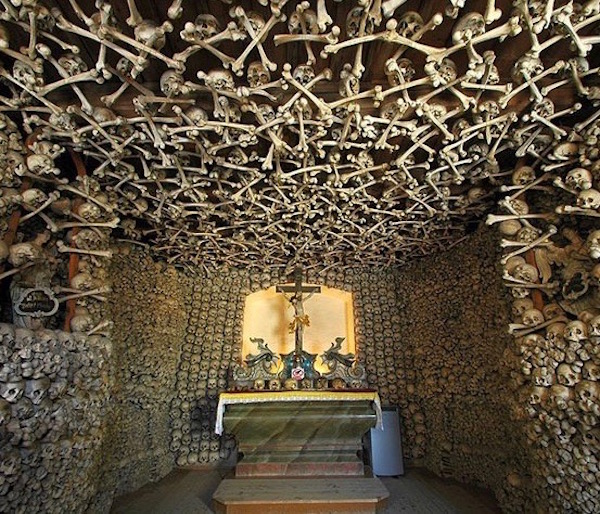
Image A
Here, bones are imaginatively and artistically arranged throughout the edifice. One of the most famous displays is a chandelier, purportedly containing every bone of the adult human body (Image B).
During the thirty years’ war, aristocracy of Central Europe wished to be buried in the hallowed graveyard at this site. As the number of burials outgrew available space, remains were exhumed and stored in the chapel, then assembled into artistic presentations.
The ruffled collars beneath the candle-bearing skulls are hip bones! At the tip-top are inverted sacra (pl.). Dangling bones are humeri (pl.). Quite the room-lighter! Makes Master Raymond’s animal skulls seem almost quaint!

Image B
Surely, these images put us in the mood to learn more about bones, although this lesson covers bones of the living. Today’s lesson will review and present more bone anatomy and types of bone cells. Then, we will cover events that ensue when bones go snap, crackle, or pop, as well as mechanisms of healing. Let’s go!
Review of Long Bone Anatomy: Lesson #39 presented long bone anatomy, but let’s take a moment to review. Once again, the femur, is our model (Image C). The shaft of a long bone is the diaphysis. The ends that form joints with other bones are the epiphyses (pl.); these are covered with articular cartilage (ball-shaped epiphysis is head of femur). The flared region between diaphysis and epiphysis is the metaphysis. Cortical bone forms a hard outer rind enclosing the marrow (medullary) cavity. Spongy bone fills epiphyses and metaphyses and is also scattered in the marrow cavity. Depending on the bone and age of the individual, the marrow cavity is filled with either fat cells or hematopoietic (blood-forming) cells, neither of which are elements of bone. Think of them as tenants not owners!
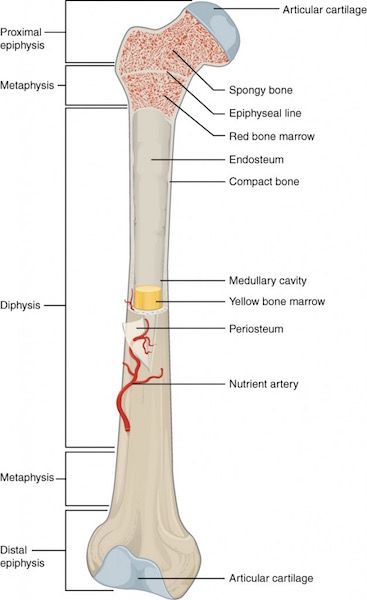
Image C
Periosteum and Endosteum: Periosteum is a thick fibrous layer covering the diaphyseal surface (Image D). Endosteum is a thin connective tissue layer lining the bone marrow cavity and covering all exposed surfaces of spongy bone. Both layers contain blood vessels and several types of bone cells as discussed below.
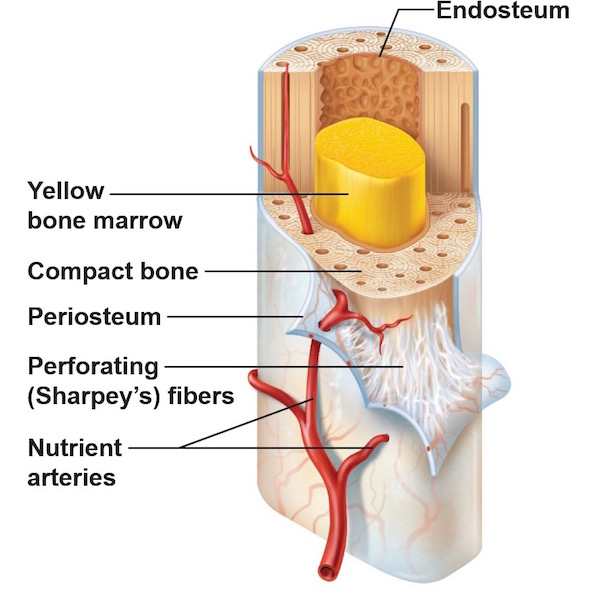
Image D
Vascular Supply: As we learned in Anatomy Lesson #39 “Dem Bones – The Human Skeleton,” bone is living tissue and thus requires a constant blood supply such that the human skeleton receives 5-10% of the entire cardiac output (amount of blood the heart pumps per minute).
To meet this demand, large bones receive several arteries (Image E). Periosteal arteries supply periosteum and outer compact bone. Epiphyseal arteries supply blood to epiphyses (pl.). Nutrient arteries supply inner cortical bone, endosteum, and help supply epiphyses and metaphyses.
These arteries access a bone via foramina (channels) that traverse compact bone to reach their respective turfs, then break into capillary beds where oxygen and nutrients are exchanged for carbon dioxide and waste products. Corresponding veins form and blood flows back to the heart. Round and round and round it goes…..
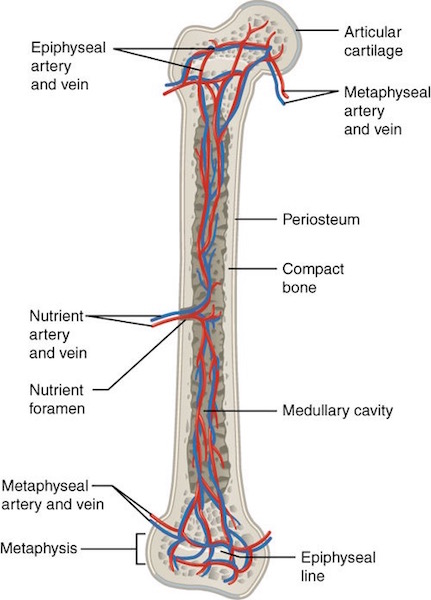
Image E
Nerve Supply: You may be surprised to learn that mineralized bone (organic matrix plus inorganic minerals – see Lesson #39) does not have pain receptors. Hum…if this is true, then why does a broken bone hurt so badly? Because periosteum and endosteum as well as articular surfaces are richly supplied with pain receptors (nociceptors). If these structures are compromised as with a fracture, then pain is severe!
Image F nicely illustrates nerve and blood vessel distribution in cortical bone and margin of the marrow cavity. Anatomy typically color codes arteries red, veins blue, and nerves yellow. The tiny yellow lines indicate that nerves follow blood vessels through cortical bone to the endosteum. Although not shown in Image D, nerves also follow periosteal arteries to innervate the periosteum.
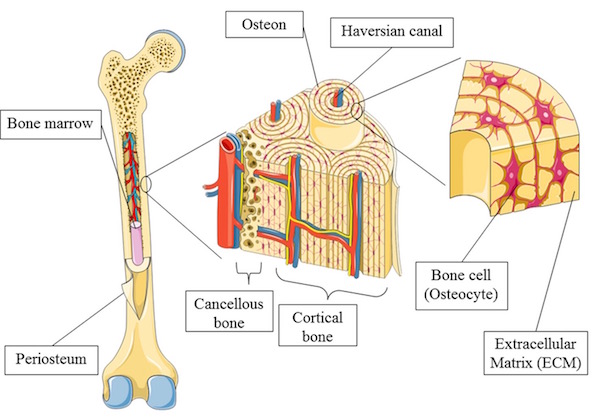
Image F
Bone Cells: As mentioned above, bone contains several cell types including osteogenic cells, osteoblasts, osteocytes, and osteoclasts (Image G). These cells are located in periosteum, endosteum, or within mineralized bone. Again, although hematopoietic cells or fat cells fill spaces between spongy bone and within marrow cavities, these are not bone cells.
Osteogenic cells are stem or parent cells giving rise to osteoblasts (Image G); they reside in periosteum and endosteum.
Osteoblasts: From Greek osteo- meaning bone + blastanō meaning to germinate, osteoblasts produce collagen and other proteins as part of the organic matrix. These proteins are released into the extra-cellular environment where minerals deposit around them. Together, the organic matrix provides tensile strength and inorganic minerals provide compressive strength. As to their bulk, organic proteins represent 10% of bone mass with the remaining 90% being inorganic mineral. Osteoblasts reside in periosteum and endosteum.
Osteocytes: In the course of production and secretion of organic matrix and its subsequent mineralization, osteoblasts become “imprisoned” within bone and are renamed osteocytes. Located in compact and spongy bone, osteocytes help maintain the mineralized bone. Further, the mineralized matrix with imprisoned osteocytes is organized into cylinders of bone known as osteons (Haversian systems). A bone such as the femur contains millions of osteons but details about these units must await a future lesson.
Osteoclasts: Giant, multi-nucleated cells, the osteoclasts, are formed by the fusion of macrophages (Anatomy Lesson # 37, “Outlander Owies Part 3 – Mars and Scars”). Found in endosteum, their duty is to dissolve bone.
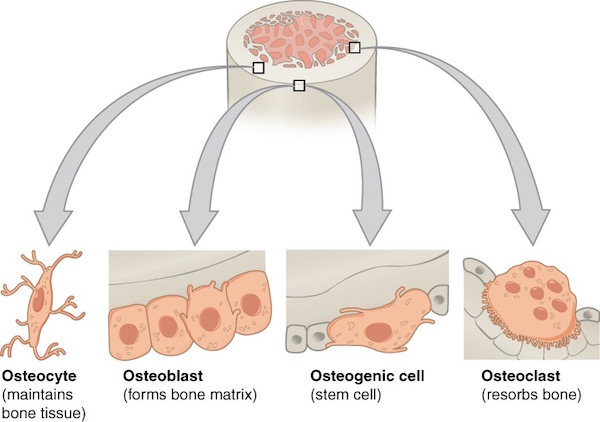
Image G
As you might imagine, a good deal of coordination among the various bone cells is required to ensure homeostasis (balance) between bone production, maintenance, and resorption. For example, as a bone grows in circumference due to periosteal osteoblast activity, osteoclasts of the endosteum remove bone from the inside so the thickness remains fairly constant, a highly regulated process.
Image H shows in detail the distribution of bone cells in periosteum, endosteum and in compact bone.
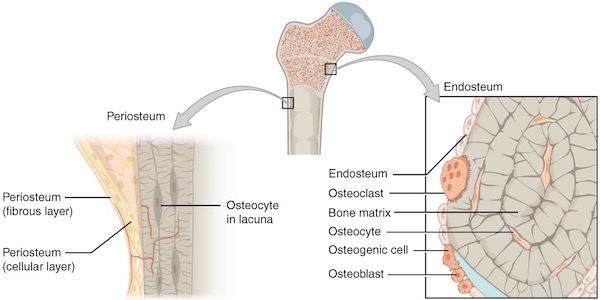
Image H
Next, let’s do something really daring and look at a microscopic image of bone cells as viewed through a light microscope (Anatomy Lesson #34 – “The Amazing Saga of Human Anatomy”). Please understand that microscopic anatomy, better known as histology (Greek histo- meaning “tissue” + ology meaning “to know”), is a challenge for most students. Watch this fun video by Harvard medical students as they lament about studying “histo!”
https://www.instagram.com/p/BEYogsIuTPz/
Ha ha! Very clever, medical students! But, you readers might respond the same way looking at a magnified image of a shard of spongy bone (Image I). This image is of a very thin slice of bone that has been stained blue and pink with H&E (hematoxylin = blue + eosin = pink). The so-called H&E stain is the most commonly-used histo stain in the US.
So, what do we see in Image I? The dense pink vertical band is a spicule of ossified spongy bone. The oval cells with pale nuclei along the left border of the shard are osteoblasts laying down a pale layer of unmineralized organic matrix (osteoid). The right border of the spicule show two large multi-nucleated osteoclasts busily dissolving bone – one such interface is a distinct divot indicated by the black arrowheads. Such divots are termed Howship’s lacunae (named for John Howship, a British anatomist). Several irregularly-shaped nuclei are scattered within the bony spicule – these are osteocytes encased in ossified bone.
That’s pretty much it! Being competent at recognizing cells and extracellular substance is based on pattern recognition. Looking at many examples of a given tissue is very useful in obtaining said competence. If you think this is impossible, understand that anatomical pathologists make their living looking at and diagnosing diseases from thousands of such tissue slides.
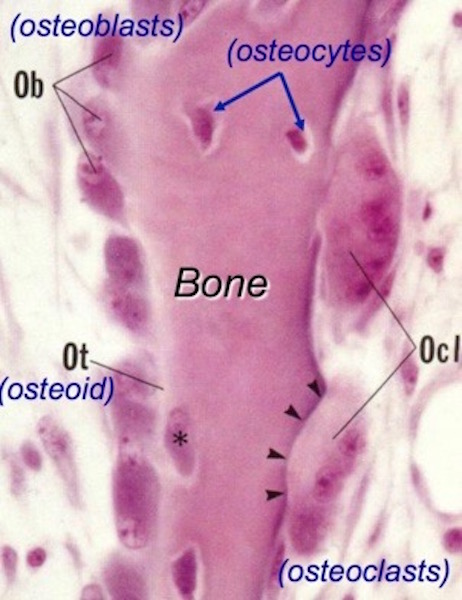
Image I
Bone Fractures: Time for snap, crackle, and pop, and I dinna mean Rice Krispies! Compressive strength from mineral deposition and tensile strength from organic matrix give normal bones the ability to behave elastically. If trauma overcomes this elasticity, then bones fracture!
Bone fractures fall into two major categories: mechanical bone fractures caused by high force impact or stress, and pathological fractures caused by disease.
Pathological Fractures: Diana presents a fabulous case of fracture caused by disease in Colum. The Laird of clan MacKenzie is haunted by the aftermath of a pathologic fracture and accompanying deformities due to Toulouse-Lautrec syndrome (Starz episode 208, The Fox’s Lair).
Outlander book informs readers that at 18 y.o., Colum took a bad fall breaking the long bone (femur) of his thigh that subsequently mended poorly. Other skeletal anomalies quickly ensued. Diana explains in Dragonfly in Amber:
Legs crippled and twisted by a deforming disease, Colum no longer led his clan into battle…
…He glanced dispassionately down at the bowed and twisted legs. In a hundred years’ time, they would call this disease after its most famous sufferer—the Toulouse-Lautrec syndrome.
Read Anatomy Lesson #27, “Colum’s Legs and Other Things too!” for details about this rare syndrome (1.7 per million births). Of course, there are also many other diseases leading to pathological fractures. Nowadays, the most common in the US is osteoporosis.

Mechanical fractures: High force impact or stress cause bones to snap. Different types of bones (e.g. short vs. long) often exhibit characteristic fractures. This lesson will consider fractures of long bones using the femur again as our example. Fractures are generalized into six different categories:
Then, fractures are named according to features of the break (Image J).
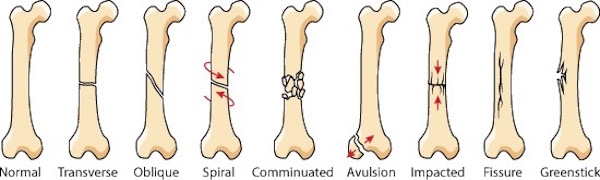
Image J
Fracture Healing: Fracture healing is the process by which the body repairs a broken bone and what a process it is! Several overlapping steps occur, different descriptors are used, and times may vary depending on the bone, but the general sequence is (Image K):
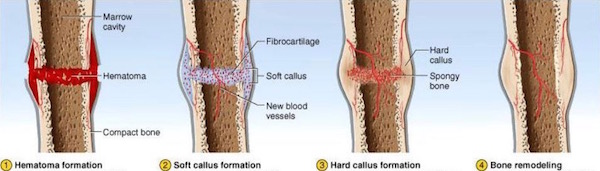
Image K
Normal fracture healing requires the following:

Image L
Now for some real “fun.” With Starz images, let’s use applied anatomy to consider mechanical bone fractures and healing. Starz Outlander episodes offer two excellent examples of bone fractures, both are compound in type.
A workman is admitted to L’Hôpital des Anges in Paris (Starz episode 204, La Dame Blanche). He screams in agony because he has suffered a compound fracture of the right tibia (Anatomy Lesson #27, “Colum’s Legs and Other Things too!”). The skin is open and the upper part of the broken tibia is clearly visible at the red arrow.
This injury hurts like holy toothpicks because tears of periosteum and endosteum stimulate nociceptors (pain receptors). Then, muscles spasm as they attempt to stabilize bony fragments, upping the pain meter. And, adding insult to injury, a compound fracture rents the skin and we all ken how sensitive skin is to pain! All around, an agonizing situation.
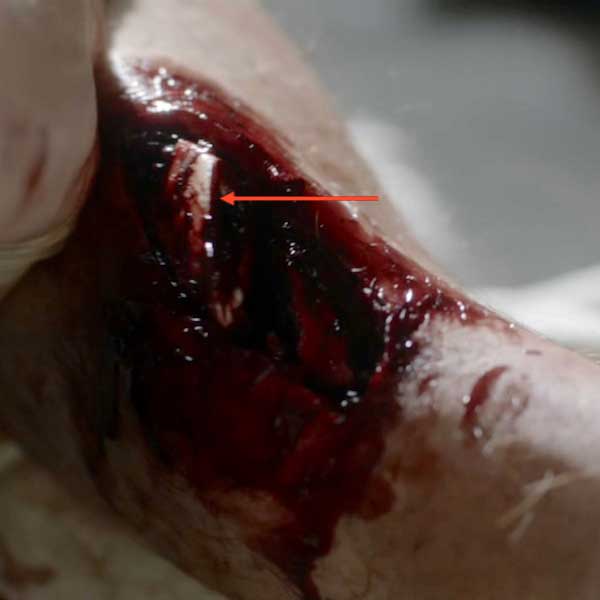
So, what does a good hangman do to ease his patient’s discomfort? Why, he hammers a nail into the side of the poor fellow’s knee, of course! What else? Presumably a type of primitive acupuncture, it momentarily halts the patient’s agony; mayhap from PTSD?
A quote from Dragonfly in Amber:
Monsieur Forez was at work today. The patient, a young workman, lay white-faced and gasping on a pallet. …The leg, though, was something else… Sharp bone fragments protruded through the skin … “Here, ma soeur ,” he directed, taking hold of the patient’s ankle. “Grasp it tightly just behind the heel… Monsieur Forez brought the point of the brass pin to bear …he drove the pin straight into the leg with one blow. The leg twitched violently, then seemed to relax into limpness.

Monsieur Forez enlightens Claire regarding this startling exhibit of bedside manner (from Dragonfly in Amber):
“There is a large bundle of nerve endings there, Sister, what I have heard the anatomists call a plexus. If you are fortunate enough to pierce it directly, it numbs a great deal of the sensations in the lower extremity.”
Stop! I must pick at a wee bone: During the episode, Mr. Forez explains to Claire that anatomists describe a nerve at the inside of the knee which, if pierced, briefly anesthetizes the leg (Anatomy Lesson #27 – “Colum’s Legs and Other Things too!”). So, the human grease-guy whacks a 4” nail into the side of the workman’s knee for pain relief!
So this is what troubles me: the nail pierces skin near the saphenous nerve (a branch of the femoral) which, unfortunately, supplies only skin of the area and does nothing for bone pain. The correct nerve to pierce would be the tibial nerve, a branch of the sciatic; but, both of these nerves are in the back of the thigh! From the thigh, the tibial nerve sends fibers to the tibia in concert with its nutrient artery where it innervates endosteum and periosteum. Ergo, for this technique to work, the good Monsieur must pierce the tibial nerve in the back of the thigh.
I canna vouch for the efficacy of nail piercing, which seems a wee bit harsh, but I can question Forez’s anatomists and their data base. Soon after the shock of piercing subsides, the patient resumes screaming so I canna think it verra efficacious. Gah! Back to the dissection lab for those anatomists! But, I must say, the special effects are superb!

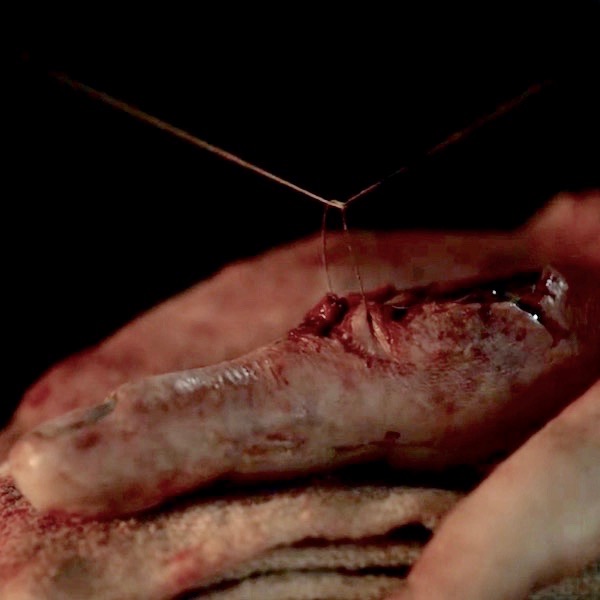
Next, we will consider another compound fracture, arguably the most infamous of the Starz series. The Wentworth Smack-Down delivered high force impact causing mechanical fractures of Jamie’s left hand bones (Starz episode 115, Wentworth Prison). Let’s do a walk through of these fractures.

Heading to Outlander book, Diana enlightens us with these quotes:
Luckily the thumb had suffered least; only a simple fracture of the first joint. That would heal clean. The second knuckle on the fourth finger was completely gone; I felt only a pulpy grating of bone chips when I rolled it gently between my own thumb and forefinger…
The compound fracture of the middle finger was the worst to contemplate. The finger would have to be pulled straight, drawing the protruding bone back through the torn flesh. I had seen this done before—under general anesthesia, with the guidance of X rays.
We can easily deduce from Diana’s description that, at a minimum, Jamie’s hand suffered:

Like any combat nurse worth her salt, Claire cleanses Jamie’s wounds. She has no modern isotonic fluids or antibiotics, so she cleans his compound fracture with (no doubt) sterile water, perhaps containing a wee dram of alcohol for sterilization?

Next, Claire ponders the damage and then re-aligns and resets the bony fragments (Starz episode 116, To Ransom a Man’s Soul). And again from Outlander book:
I began to lose myself in the concentration of the job… deciding how best to draw the smashed bones back into alignment.

Now, as we learned above, a compound fracture tears surrounding flesh and skin. So Claire carefully closes the wounds with sutures (Starz S.2, introductory image) to exclude pathogens and reduce blood loss.
Earlier in this lesson, we read that movement of a new fracture interferes with callus formation. So, various devices are used to immobilize fractures as they heal.
Ever resourceful Claire (or the monks?) devises an external fixator for Jamie’s smashed hand in the form if a very clever wire/leather, linen, and wood device! External fixation is a surgical treatment used to stabilize bone and soft tissues at a distance from the injury. So, check out the amazing invention (Starz episode 116, To Ransom A Man’s Soul) to immobilize Jamie’s hand! The middle finger is reset and stitched. The communiated and most severely wounded ring finger is stitched and splinted against the small finger. Brava, Madam Sassenach!

Jamie’s hand care is not yet complete! Claire provides physical therapy in the form a rag ball she made. Squeezing the ball helps Jamie regain hand mobility and strengthen the knitting bones as he and Murtagh plan how best to skewer BJR (Starz episode 203, Useful Occupations and Deceptions)!
In case you forgot from earlier in this lesson, exercising a repairing bony callus augments the ossification process, so Claire’s rehabilitation plan is spot on!
Two quotes from Diana’s Dragonfly in Amber:
It really wasn’t too bad; a couple of fingers set slightly askew, a thick scar down the length of the middle finger. The only major damage had been to the fourth finger, which stuck out stiffly, its second joint so badly crushed that the healing had fused two finger bones together. The hand had been broken in Wentworth Prison, less than four months ago, by Jack Randall.
He had regained an astounding degree of movement, I thought. He still carried the soft ball of rags I had made for him, squeezing it unobtrusively hundreds of times a day as he went about his business. And if the knitting bones hurt him, he never complained.

And, pithy quotes from Diana’s Dragonfly in Amber remind us that months later, Jamie’s hand is still not whole (Starz Season 2 opening images), so clever caring Claire applies her personal version of massage therapy… a task that she and he undoubtedly relish! Hee, hee.
I crawled in beside him and took up his right hand, resuming my slow massage of his fingers and palm. He gave a long sigh, almost a groan, as I rubbed a thumb in firm circles over the pads at the base of his fingers.

Thus ends Outlander compound fractures and healing. Whether bone breaks or skeletons, people are endlessly fascinated by bones and the stories they tell. Book readers will recognize this poignant commentary from Dragonfly in Amber as Jamie and Claire find the bony inhabitants of an unknown cave in France.
He turned again then to the two skeletons, entwined at our feet. He crouched over them, tracing the line of the bones with a gentle finger, careful not to touch the ivory surface. “See how they lie,” he said. “They didna fall here, and no one laid out their bodies. They lay down themselves.” His hand glided above the long arm bones of the larger skeleton, a dark shadow fluttering like a large moth as it crossed the jackstraw pile of ribs.
Now, I have my own bone story to share. The following is a true event underscoring the amazing capacity of bones to heal. During WW II, my father was a welder of Liberty Ships in California. When I was 18 months of age, neighborhood kids accidentally ran over me and the trauma snapped off the head (ball-shaped epiphysis) of my right femur. Local physicians were unable to help so they sent us to the Treasure Island Naval Base where many of the best US physicians were stationed to assist with the war effort.
Those docs had never set a child’s femoral head before, but they courageously reset my leg, placed me in a 3/4 body cast, and prepared my parents for the bad news: the blood supply to the femoral head was likely severed, the femoral head would become necrotic (die), and the hip would freeze into an immobile joint. I would not walk normally, if at all.
Well, the good news is that my femoral head did not perish! Somehow and somewhere, an arterial supply survived. Although my colleagues and I share theories about which vessel might have remained intact, no one knows for sure.
Image M was taken in 1944 at Stinson Beach, CA, six months after the injury (like the artery, my appetite clearly remained intact <G>). Observe that the right leg is slightly rotated outward (externally), a classic stance following a femoral head fracture.
Today, the only residual is my right leg is 3/8” shorter than the left. Otherwise, nada! I am able to exercise vigorously and with no noticeable deficit. Blessings to those unknown healers who helped the wee bairn of a common laborer!

Image M
Our lesson on how fractures heal has come to an end. After two lessons about the skeleton, there remains much more to be studied, so we may revisit this topic at a later date.
A few last thoughts: Remember, bone is a dynamic tissue which constantly remodels itself throughout life. Individual bones are organs that collectively constitute the skeleton, our internal support system. Bone cells create, maintain, and destroy bone tissue to our benefit.
Bones have been prodded, examined, healed, revered, saved, feared, embellished, and cherished. Not all of this lesson is about happy stuff, so let’s end with this slightly irreverent image from the bow of the Titanic.

Image N
Dem bones, dem bones!
A deeply grateful,
Outlander Anatomist.
Photo creds: Starz, Outlander Anatomy archives (Image M), www.anatomy-medicine.com (Image F), www.askabiologist.edu (Image J), www.apps.carleton.edu (Image B) www.boneandspine.com (Image C), www.geneticliteracyproject.org (Image L), www.medcell.med.yale.edu (Image I), www.reddit.com (Image A), www.en.wikipedia.org (Image E; Image H), www.everythingfunny.org (Image N), www.commons.wikimedia.org (Image G) ,www.studyblue.com (Image D), www.ippe2ools.blogspot.com (Image K)
Hello, anatomy students! Today’s Anatomy Lesson #37 covers the ginormous topic of mars and scars, better known as wound healing. A mess of wounds and scars appear in the Outlander books and the Starz series so let’s learn from this perfect anatomical smorgasbord.
You will recall from Anatomy Lesson #35: Outlander Owies! Part One and Anatomy Lesson #36: Outlander Owies! – Part Deux! that pathology is the study of abnormal anatomy. Well, it turns out that wound healing also belongs in the realm of pathology. Our lesson will examine healing of closed and open wounds.
Surprise! Jamie is our model because he has more mars and scars than anyone else of Outlander fame! Let’s also enjoy a drinking game because Jamie’s wounds inspire one to drink more than any others, I ken! Down a wee dram each time you read “Och! Jamie’s puir…”
Drams in hand? Let’s begin…
Blood: Because blood is essential for healing and scar formation, it requires a brief brief mini-lesson of its own. Blood is a connective tissue (yes, it is!) composed of fluid plasma, in which two classes of blood cells are suspended: red blood cells (RBCs or erythrocytes) and white blood cells (WBCs or leukocytes). Blood also contains cell fragments known as platelets (thrombocytes) along with many other suspended or dissolved substances.
RBCs arise in bone marrow as nucleated cells but lose their nuclei just before entering the blood stream. Image A shows a 3-D SEM (Scanning Electron micrograph, Anatomy Lesson #34) image of a blood vessel containing blood cells. Understand that the colors in Image A were computer generated. RBCs are flat, biconcave discs (red in Image A), whose shape and lack of a nucleus allots them maximum oxygen-carrying capacity; think of them as tiny flat bags filled with hemoglobin (Hgb). As RBCs pass through lung capillaries, oxygen binds to Hgb molecules, turning RBCs bright red. As RBCs reach capillaries of other body regions, Hgb molecules release their oxygen burden into the tissues and the RBCs turn a dark, deep red color. Such color changes are important in wound formation and healing.
WBCs are the round, gray fluffy balls in Image A. They arise in bone marrow but retain their nuclei. There are five classes and several subclasses of WBC. All WBCs serve various defensive functions; more about these later in the lesson.
Platelets, which do not appear in Image A, play a crucial role in blood clotting.
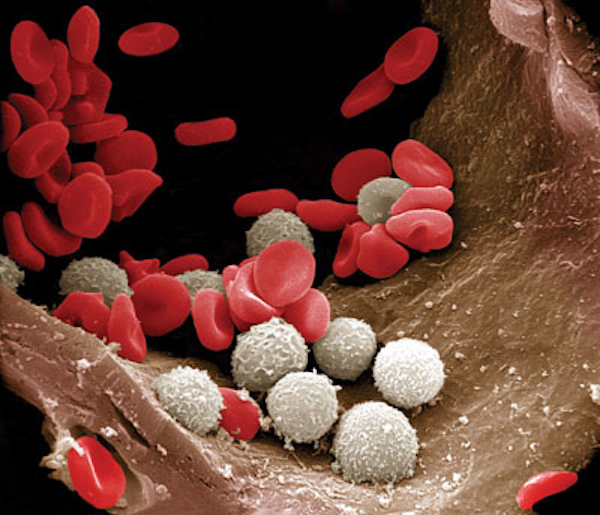
Image A
That was a “quickie” blood lesson. Now, on to healing processes!
The outline for today’s Lesson is:
Healing Closed Wounds: Closed wounds are injuries wherein the skin remans unbroken. The contusion will serve as today’s example of a closed wound, although simple bone fractures are another. Anatomy Lesson #35 explained that a contusion is the medical term for a bruise. Bruises form in subcutaneous tissues (Anatomy Lesson #5: “Claire’s Skin” – “Ivory, Opal and White Velvet.”) where they are often visible through the skin, but they can also form in deep organs such as muscle. Symptoms may include a bump, a hard knot and tenderness. And, bruises do not blanch under pressure. A number of steps occur to form and heal a bruise including:
Let’s look at each of these steps.
Trauma: Contusions are caused by blunt force trauma wherein the skin is not broken. Claire’s foot presents an formidable blunt force directed at Jamie’s face (Starz episode 109, The Reckoning)! Weil, now, she did warn him not to belt her. This lass is not going down without a stramash!

Contusion Development: Contusions pass through an impressive array of colors during development and healing. The first color is redness which occurs because blunt trauma bursts local capillaries allowing oxygen-ladened RBCs (bright red) to spill into nearby tissues. Although time has passed since Claire’s kick, the skin overlying Jamie’s right bony orbit (Anatomy Lesson #30: Aye, Eye – The Eyes Part 2!) shows the redness typical of a fresh contusion (Starz episode 110, By the Pricking of My Thumbs). Or, mayhap he is just blushing because the Duke of Sandringham has a certain fondness for his hindquarters? <G> Och! Jamie’s puir right eyelid! Have a wee dram.
Redness is followed by purple and blue discoloration as Hgb molecules inside the spilled RBCs release their oxygen; the RBCs turn dark red-purple as do the tissues they occupy. Next image is a good example of purple/blue discoloration (Starz episode 116, To Ransom a Man’s Soul). Och! Jamie’s puir left shoulder! (And, another dram). A quote from Outlander book reminds us of the vicious swipe that produced such discoloration!
The spot on his left side where the mallet had struck was an ugly contused swelling…I bit my lip, feeling gingerly down the swell of his biceps. He had one of the worst bruises I had ever seen; a huge mottled splotch of purple-blue—but I was fairly sure the arm wasn’t broken.

Next, a contusion exhibits the classic black and blue discoloration as spilled RBCs rupture and release their iron-containing Hgb into the soft tissues of the injured area. Och! Jamie’s puir left fingers; they argued with that damnable mallet and lost (Starz episode 116, To Ransom a Man’s soul)! Quick! Take another sip!
Contusion Resolution: Yay! It rhymes! Now, the contusion begins to heal assuming first, green and then, yellow hues. These color changes occur because cells known as macrophages (Greek makros meaning large + phagein meaning to eat) devour freed Hgb, Macrophages break the Hgb into the green compound, biliverdin, (Latin meaning green) which turns the tissues an icky green color. This is followed by yellow hues as the biliverdin is metabolized into the golden chemical, bilirubin. As macrophages clear the last of the debris from the bleed, the yellow fades and if the contusion isn’t too profound, normal coloration and function are restored.
Ergo, changes oin Hgb molecules form the basis for color changes of a healing contusion. A single bruise can simultaneously display all of the above colors because the amount of spilled blood varies in different areas and the stages of healing overlap. Here is a gut-wrenching example (Starz episode 106, The Garrison Commander)! Och! Jamie’s puir back! (Another swallow!) Gah! Skin near the lash marks is red, purple, blue, black, green, and yellow! Herself writes in Outlander book:
Dougal grimaced. “A pitiful sight, it was, too—still raw, no more than half-healed, wi’ the weals turned black and the rest yellow wi’ bruises. The thought of a whip comin’ down on that soreness was enough to make me blench, along wi’ most of those watching.”
Now that we understand the healing of a closed wound, let’s consider open wounds.

Open Wound Healing: Open wounds entail skin breaks; abrasions, lacerations, and incisions (Anatomy Lesson #35) are good examples of open wounds. Such injuries undergo a cascade of events during wound healing.
Trauma: First, open wound healing requires trauma; finding good examples of open wounds in Outlander is a no-brainer – as they are pretty much everywhere! This is a fine one: Starz episode 110, By the Pricking of My Thumbs, shows the type of trauma-drama awaiting highlanders that mess with Jamie! The MacDonald lads hurl nasty insults and then attack Jamie. Thalla gu h-Iort – “to St Kilda with ye!” bellows Jamie. With a quick dirk-jerk, Jamie gifts one lad with an incision of his right hamstring tendons! Young MacDonald came to harm, E-I-E-I-Oooooh; that stings!

Open wound healing: Following trauma, the body immediately springs into action and initiates the following four steps of open wound healing (Image B):
Wake up, students! Let’s examine each of these four steps.
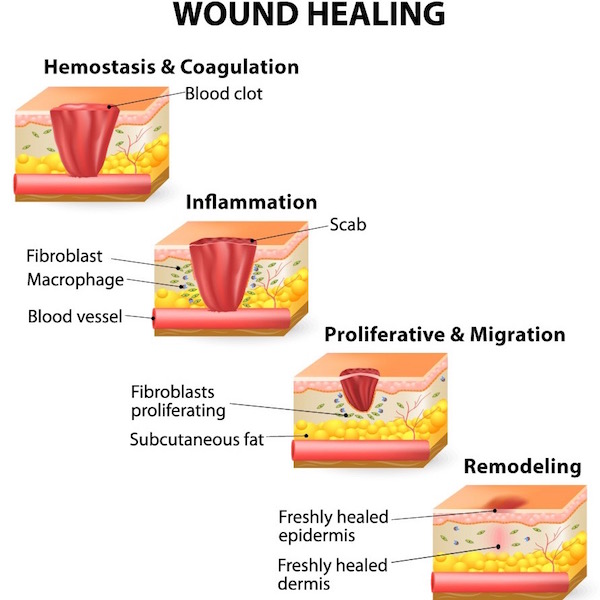
Image B
Hemostasis: A fancy word for blood clot, hemostatsis comes from the Latin for blood + Greek for stop. Hemostasis is typically the first step in open wound healing. If trauma ruptures blood vessels, they bleed (duh!) and then undergo spasm to reduce bleeding. Next, platelets stick to the injured site forming a temporary platelet plug, followed by a complex, ten-step!!! cascade of events leading to blood clot formation. If all steps work normally, a clot stoppers each damaged blood vessel to halt blood loss. The dusky red plug of Jamie’s gunshot wound is a massive blood clot formed by the process of hemostasis (Starz episode 101, Sassenach). Och! Jamie’s puir right trapezius muscle! Slàinte!
And, just to keep us honest and abreast of Outlander time line, a common 17-century word for blood clot is grume!

A blood clot with its seeping fluids usually hardens into a scab, the body’s version of a Band-Aid! This firm shell protects the wound from infection and desiccation (drying). Tissues under a scab are repairing so best to leave it alone. If you pull it off, the healing process will be prolonged. Jamie kens better than to tear that scab off his gunshot wound! Nurse Claire will skelp his arse if she catches him doing that (Starz episode 103, The Way Out) From Outlander book:
“That’s good,” I said, clearing my throat of some obstruction that seemed to have lodged there. “It is healing well; it’s scabbed over nicely, and there’s no drainage at all. Just keep it clean, and don’t use the arm more than you must for another two or three days.” I patted the undamaged shoulder, signifying dismissal.

Inflammation: Hemostasis is quickly followed by acute inflammation, a rapid but brief response that is not the same as infection, although both may occur simultaneously. Just so you know, the body also experiences chronic inflammation (e.g. RA), a prolonged response that lies beyond today’s lesson content. So, let’s investigate acute inflammation.
About 2,000 years ago, the Roman, Celsus, described four signs of acute inflammation (rubor, tumor, calor, dolor). The fifth sign (functio laesa), was described centuries later by Rudolf Virchow, father of modern pathology. The signs, in Latin followed by their English equivalents, are:
Acute inflammation is the topic of a terse tête-à-tête between Mrs. Fitz and newly arrived Claire (Starz episode 102, Castle Leoch). Claire declares she doesn’t want Jamie’s gunshot wound to become infected. Oops, she means inflamed! Why did Claire change her words? Because, she kens that the terms infected/infection, meaning invasion by micro-organisms, will not be accepted for another 140 years or so! Herself enlightens us from Outlander book:
“But he’s hurt. He was shot yesterday and stabbed last night. I bandaged the wound for riding, but I didn’t have time to clean or dress it properly. I must care for it now, before it gets infected.” “Infected?” “Yes, that is, I mean, inflamed, you know, with pus and swelling and fever.” “Oh, aye, I know what ye mean. But do ye mean to say as ye know what to do for that? Are ye a charmer then? A Beaton?” “Something like that.”
Hee, hee – more like a WW II combat nurse. If only Mrs. F. knew!

The five signs of acute inflammation are caused by dramatic changes in small blood vessels, WBC distribution, and chemical mediators. These changes are very complex so suffice it to say that intact blood vessels near the injury become leaky such that plasma and some types of WBCs pour into the injured tissues. The increased blood flow causes redness. Leaked plasma causes swelling. Freed WBCs release chemical mediators that initiate a host of tissue changes including more redness, swelling, pain, and heat. These responses are designed to eliminate the cause of cell injury, to remove damaged cells, and to initiate tissue repair. Because the injured area hurts, it is hard to use, so it undergoes loss of function. Got it? Grand!
Back to the present (or past): here’s a great example of an injury that leads to acute inflammation. Just before Jamie’s dirk-jerk, he is stabbed by one the MacDonald lads during the big Mac-Attack (Starz episode 110, By the Pricking of My Thumbs). Och! Jamie’s puir left side! Time for another swallow!

Turning to Claire for a wee bit of TLC (she isna very accommodating) and suturing…well, at least he gets stitched <G>, we see signs of acute inflammation in Jamie’s wound (Starz episode 110, By the Pricking of My Thumbs)? See the redness? See the puffy, swollen wound margins? It hurts even before not-a-closed-mouth-woman, Claire, jabs him with her needle! And, the wound will feel warm to the touch. Och, Jamie’s puir inflamed incision wound! Getting dizzy yet?
Four of the five cardinal signs of acute inflammation accounted for! Where’s the fifth?

Here’s the fifth sign of acute inflammation: Jamie grips his newly-stitched left side to protect and support it as Colum gives the Highlanders Holy Hell (Starz episode 110, By the Pricking of My Thumbs)! This is loss of function: the wound hurts too much to use and the pain is intended to stop the victim from using the wounded area while it heals. Och! Jamie’s puir left side! Another gulp! All five signs of acute inflammation present and accounted for! Now back to the steps of wound healing.

Proliferation: So, the wound has bled and is inflamed, what’s next? The wounded tissues undergo proliferation, a complex process (yes, another one) involving three parts: angiogenesis, fibroplasia, and re-epithelialization (Image C). Whew – more terms! What do these words mean?
Angiogenesis means that new blood vessels grow into the wounded site to supply the healing tissues with oxygen and nutrients and remove waste products (red arcs and loops in Image C).
Fibroplasia means that fibroblasts (connective tissue cells) make gobs of new collagen and other structural proteins to fill the gap left by an open wound. Although laid down in a haphazard fashion, the new collagen fibers provide a structural framework for the repairing tissues (represented by ellipsoid cells and brown and yellow stacks in Image C).
Re-epithelialization means that new epidermis (Anatomy Lesson #5: Claire’s Skin – Ivory, Opal and White Velvet and Anatomy Lesson #6: Claire’s Hair – Jamies Mane or Jesus H. Roosevelt Christ!) regrows to cover the gap caused by the wound (green bricks in Image C). This fascinating step requires old epidermal cells to divide and new epidermal cells to crawl over and cover the breach (blue bumps in Image C). Then, fibroblasts (acting like muscle cells), grip the wound edges and contract, pulling the rim inward and puckering it (not shown in Image C).
If the wound is minor, the three steps of proliferation occur rapidly and the wound closes with little trace. If the wound is deep and/or wide, then proliferation results in a scar (see below).
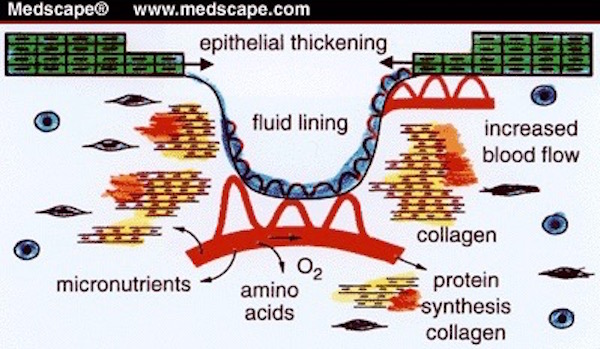
Image C
Remodeling: Finally, we arrive at remodeling, the fourth step of wound healing! Here, the randomly-arranged proliferated collagen is replaced with new collagen fibers that add strength by orienting along stress lines. Near the end of remodeling, scars contract and become smaller and paler. Image D shows that remodeling takes between 21 days for a minor wound and up to 2+ years for significant injuries! NOTE: This graph skips bleeding as the first step in open wound healing.
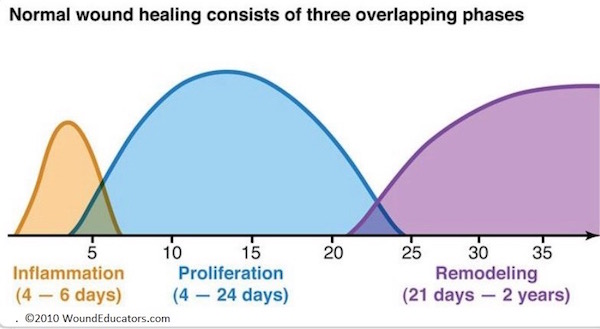 Image D
Image D
Necrosis: Before we move to scars, please know this…..If some process interferes with establishment or maintenance of normal blood flow following open wound injury, then injured tissues may undergo cell death, a process known as necrosis.
Scars or Cicatrix: We’ll end this lesson with a discussion about scars, the remnant of a healed wound. The Latin (medical) term for a scar is cicatrix or cicatrice, and has been around since the 17th century. Scars (pl.) are known as cicatrices. With the exception of minor injuries, all wounds (e.g. accident, disease, surgery) result in some degree of scarring. We are familiar with scars of the skin but did you know that our internal organs also scar and the nature of such scars is often organ-specific (e.g. fibrosis of liver).
Let’s address some common wound and scar questions.
Why are wounds stitched? Nowadays, wounds are stitched, stapled, glued, and taped. These processes align and hold together the edges of a wound to minimize bleeding, exclude infectious organisms, and reduce scar size. First recorded in 3,000 B.C., suturing is the oldest of these procedures. Approximating the edges of a wound by any the above methods permits healing by first intention.
Claire’s careful needlework on Jamie’s smashed fingers approximates his lacerated skin and restores it’s continuity, thus promoting healing by first intention and minimizing scar formation (Starz episode 116, To Ransom A Man’s Soul). She also uses interrupted stitches so if one knot releases, the entire line of stitching does not unravel. Och! Jamie’s puir left fingers! Gulp! Gasp!

Claire stitches Jamie up so many times, she might have welcomed help from this amazing little fellow!
What is the red, grainy “stuff” that fills gaping wounds? If the edges of a wound remain agape or the epidermis is gone (think floor burn), then the gap fills with granulation tissue; this red, grainy “stuff” is a combination of new blood vessels and new collagen. Known as healing by second intention, this type of healing is slower than healing by first intention and usually forms larger scars (Image E).
 Image E
Image E
Have you heard the term, “proud flesh” (caro luxurians)? Noooo, I dinna mean the Kardashians, snort! Proud flesh is an oldish term for excess granulation tissue. Image F shows proud flesh, an overgrowth of granulation tissue that developed from a small finger cut. Such overgrowths are atypical but the image is useful because it clearly shows the red blood vessels and grainy appearance of granulation tissue.

Image F
What is a scar? Scar tissue is remodeled collagen fibers that aligned in one direction for added strength. Unfortunately, scar tissue is not as functional as the tissue it replaces. For example, scar tissue of skin lacks hair follicles and sweat glands (Anatomy Lesson #6: Claire’s Hair – Jamies Mane or Jesus H. Roosevelt Christ!) and is less pliable than normal skin. Scars of heart muscle lead to loss of muscular power during cardiac contractions. Scars of liver are due to death of liver cells and formation of excess collagen – less tissue to preform the ten life-giving functions carried out by the liver. Then, there’s amazing bone that often heals without any structural or functional loss.
Why do scars turn white? Scars usually turn white within a year or two after injury. They do so after collagen remodeling and scar contraction is complete and the need for increased blood flow has diminished.
Why do some scars remain red or purple for a long time? Scars remain red or purple as long as WBCs of the area produce chemical messengers to promote increased blood flow. Thus, it may be months or even years before redness completely fades. A good example is the persistent redness of Jamie’s gunshot scar which is apparent months after the event. Oh, no! More sass from Claire who gives him a thorough Sassynach scolding for being a lousy laird (Starz episode 112, Lallybroch). Have ye ever seen a sweeter, more innocent face? Ha, ha! He enjoys a good tongue lashing now and then (hee hee!).

Here is a great … ah, erm, … I forgot what I was writing about! Gah! Oh, I remember! The scar from the sword swipe is white at the millpond even though Jamie’s earlier gunshot scar is red in the same episode (Starz episode 112, Lallybroch). Ahem, students!! The red arrow helps focus your attention on the white scar! Now this can occur because tissues in different regions of the skin may heal at different rates. More likely, it is because that bloody freezing burn contracted Jamie’s skin capillaries: reduced blood flow = paler skin! Och, Jamie’s puir left side! Are we woozy yet?

Why are Jamie’s lash scars so prominent? Back skin is thick and when lacerate, it should be sutured or stapled; unfortunately, neither of these procedures were available to Himself at the time of injury. His deep, wide lash wounds filled with granulation tissue and healed by second intention so the resultant scars are wider and more significant. BTW, his lash scars are also shiny and raised, features of hypertrophic scars, an abnormal healing process due to overproduction of collagen. His lash scars were probably designed for dramatic effect, as Jamie’s skin is an unlikely candidate for hypertrophic scarring. Och! Jamie’s puir back! Glass refill STAT!

Jamie appears over and over in this lesson because the lad has suffered more than his fair share of mars and scars. Who is to blame for most of these owies? Why, that dark, dastardly devil, BJR, of course. Claire is constantly cleaning up that SOB’s messes! Sadist that he is, Jack-Jerk finds his handwork compelling and erotic (Starz episode 116, To Ransom a Man’s Soul)! Writer Ira Steve Behr explains:
To me, the line that was truest to Black Jack’s character was when he ripped open Jamie’s shirt and said with wonder, “How does it feel to be alive and wear so much dead flesh?”
I go on record as stating, au contraire, repugnant, reptilian Randall! Scars are NOT dead flesh, they are living tissue, the end game of the body’s ability to heal wounds. Scars are molded by our own private first responders; tiny “robots” that dart into action on our behalves. Let us be grateful that our bodies possess such marvelous repair mechanisms!

Shakespeare once wrote, “There’s nothing good or bad, but thinking makes it so” (Hamlet; Act two, Scene two, p. 11). Apparently Will never met BJR – as some handiwork is just plain E-V-I-L!
If you have yet to witness this riveting compilation of Black Jack’s dark and dirty deeds, watch this admirable video – created by Julia LaBlanc and posted by E. Jamie via YouTube. Just keep in mind it grimly showcases the depths of BJR’s depravity.
https://m.youtube.com/watch?v=6GRAsvTFH4s
Closing with my own wee Ode to BJR:
BJ is a fiendish auld cur; a fiendish auld cur is he,
He called for his whip and he called for his brand,
To abuse our darling Jamie!
(Git yer foul tongue off him!)
Hope you are still standing after all those drams! As for me: Hic! Thud!
A deeply grateful,
Outlander Anatomist
Photo creds: Starz, www.bioloby-igcse.weebly.com (Image A – SEM of blood cells), www.medscape.org (Image C – proliferation), www.surpassinc.com (Image B – four steps of wound healing), www.en.wikipedia.org (Image F – proud flesh), www.woundeducators.com (Image D – phases of wound healing), www.wisegeek.com (Image E – granulation tissue)